A paper from the Weinberg Lab indicates that inflammation may be a factor in how metastatic cancer cells, those that have broken away from the original tumor, can erupt into a frenzy of growth and division months, years, or decades after initial treatment, seeding new, life-threatening tumors.
Shafaq Zia | Whitehead Institute
September 3, 2025
This migration of cancer cells, called metastasis, is especially common in breast cancer. For many patients, the disease can return months—or even decades—after initial treatment, this time in an entirely different organ.
Whitehead Institute Founding Member Robert Weinberg, also the Daniel K. Ludwig Professor for Cancer Research at Massachusetts Institute of Technology (MIT), has spent decades unraveling the complex biology of metastasis and pursuing research that could improve survival rates among patients with metastatic breast cancer—or prevent metastasis altogether.
In their latest study, Weinberg, postdoctoral fellow Jingwei Zhang, and colleagues ask a critical question: what causes these dormant cancer cells to erupt into a frenzy of growth and division? The group’s findings, published Sept. 1 in The Proceedings of the National Academy of Sciences (PNAS), point to a unique culprit.
This awakening of dormant cancer cells, they’ve discovered, isn’t a spontaneous process. Instead, the wake-up call comes from the inflamed tissue surrounding the cells. One trigger for this inflammation is bleomycin, a common chemotherapy drug that can scar and thicken lung tissue.
“The inflammation jolts the dormant cancer cells awake,” Weinberg says. “Once awakened, they start multiplying again, seeding new life-threatening tumors in the body.”
Decoding metastasis
There’s a lot that scientists still don’t know about metastasis, but this much is clear: cancer cells must undergo a long and arduous journey to achieve it. The first step is to break away from their neighbors within the original tumor.
Normally, cells stick to one another using surface proteins that act as molecular “velcro” but some cancer cells can acquire genetic changes that disrupt the production of these proteins and make them more mobile and invasive, allowing them to detach from the parent tumor.
Once detached, they can penetrate blood vessels and lymphatic channels, which act as highways to distant organs.
While most cancer cells die at some point during this journey, a few persist. These cells exit the bloodstream and invade different tissues—lungs, liver, bone, and even the brain—to give birth to new, often more aggressive tumors.
“Almost 90% of cancer-related deaths occur not from the original tumor but when cancer cells spread to other parts of the body,” says Weinberg. “This is why it’s so important to understand how these ‘sleeping’ cancer cells can wake up and start growing again.”
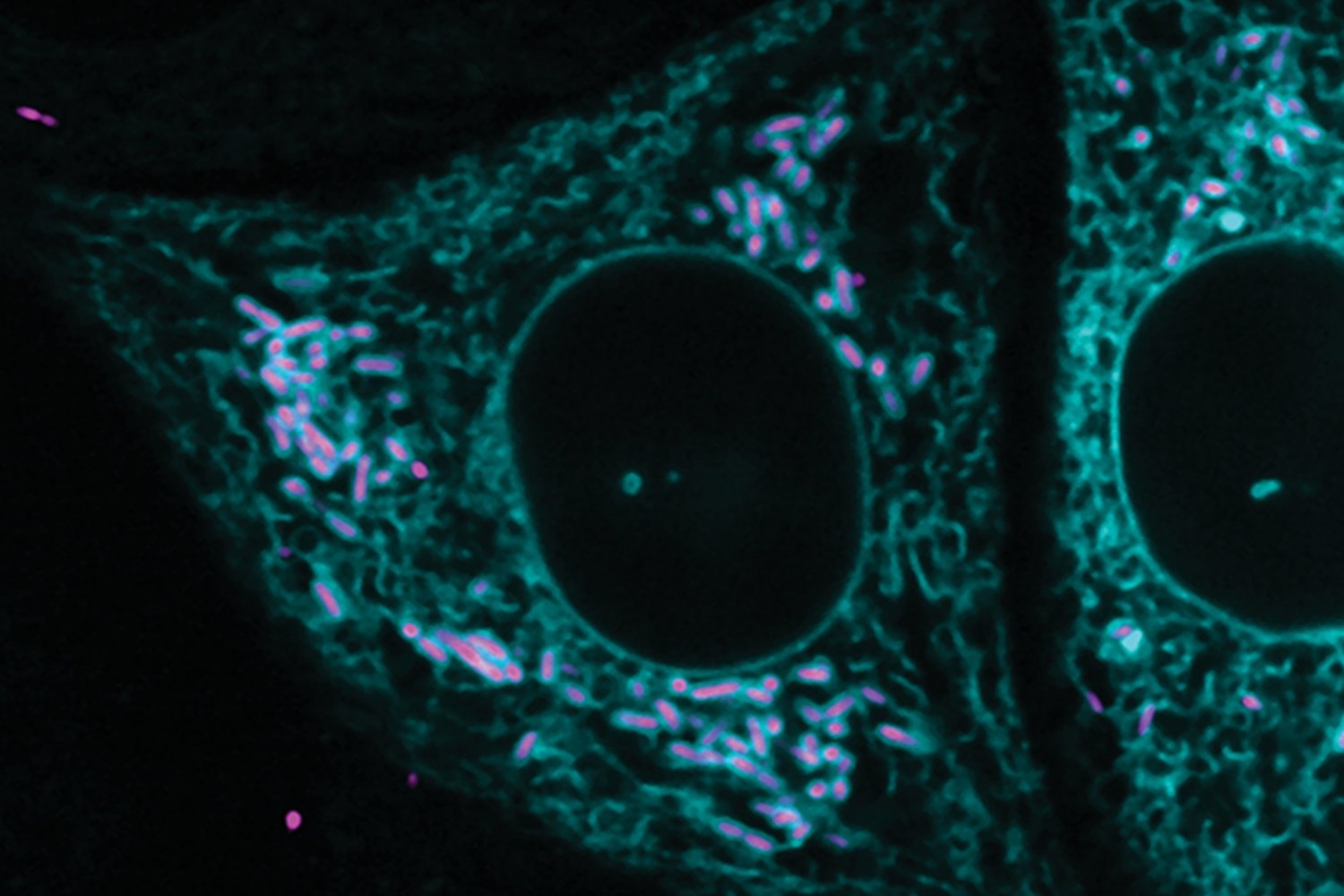
Setting up shop in new tissue comes with changes in surroundings—the “tumor microenvironment”—to which the cancer cells may not be well-suited. These cells face constant threats, including detection and attack by the immune system.
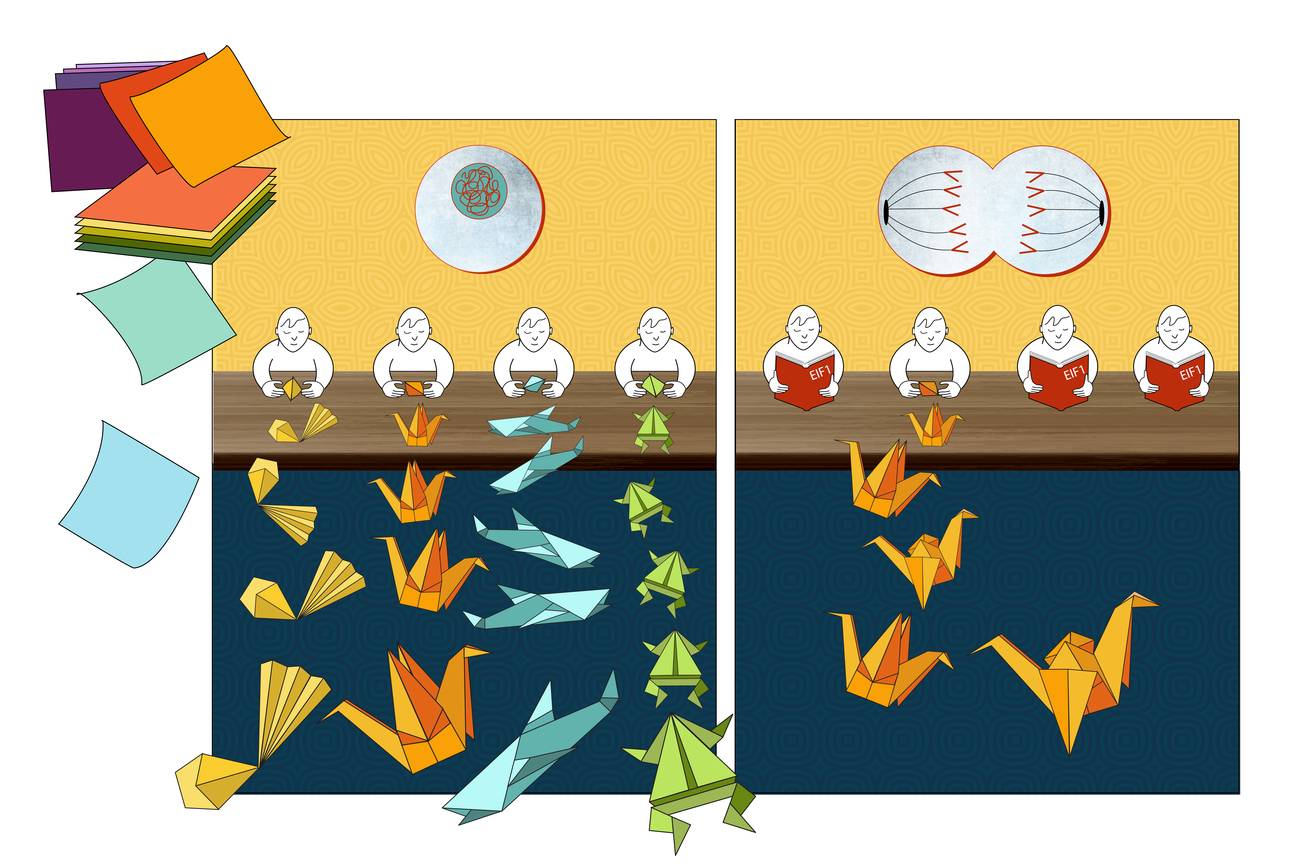
To survive, they often enter a protective state of dormancy that puts a pause on growth and division. This dormant state also makes them resistant to conventional cancer treatments, which often target rapidly dividing cells.
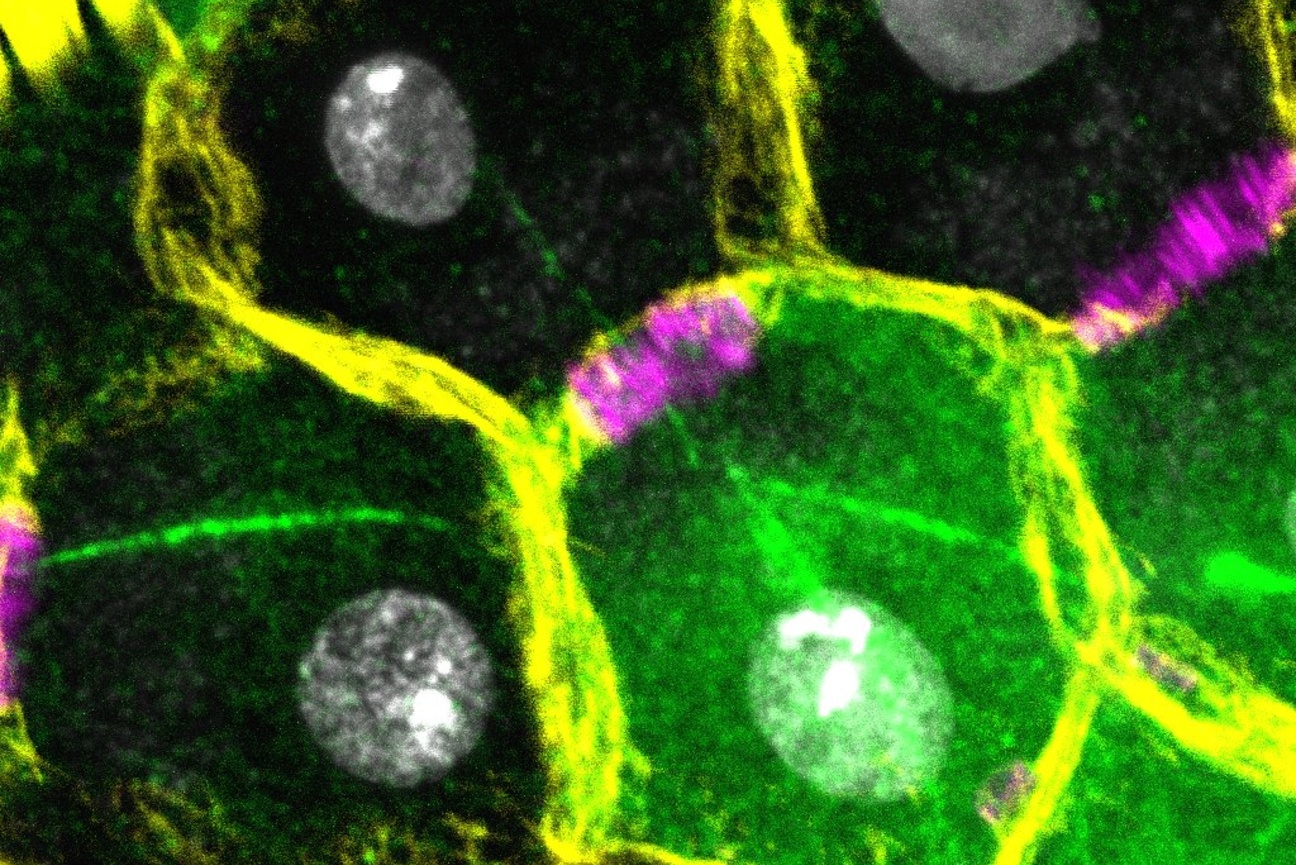
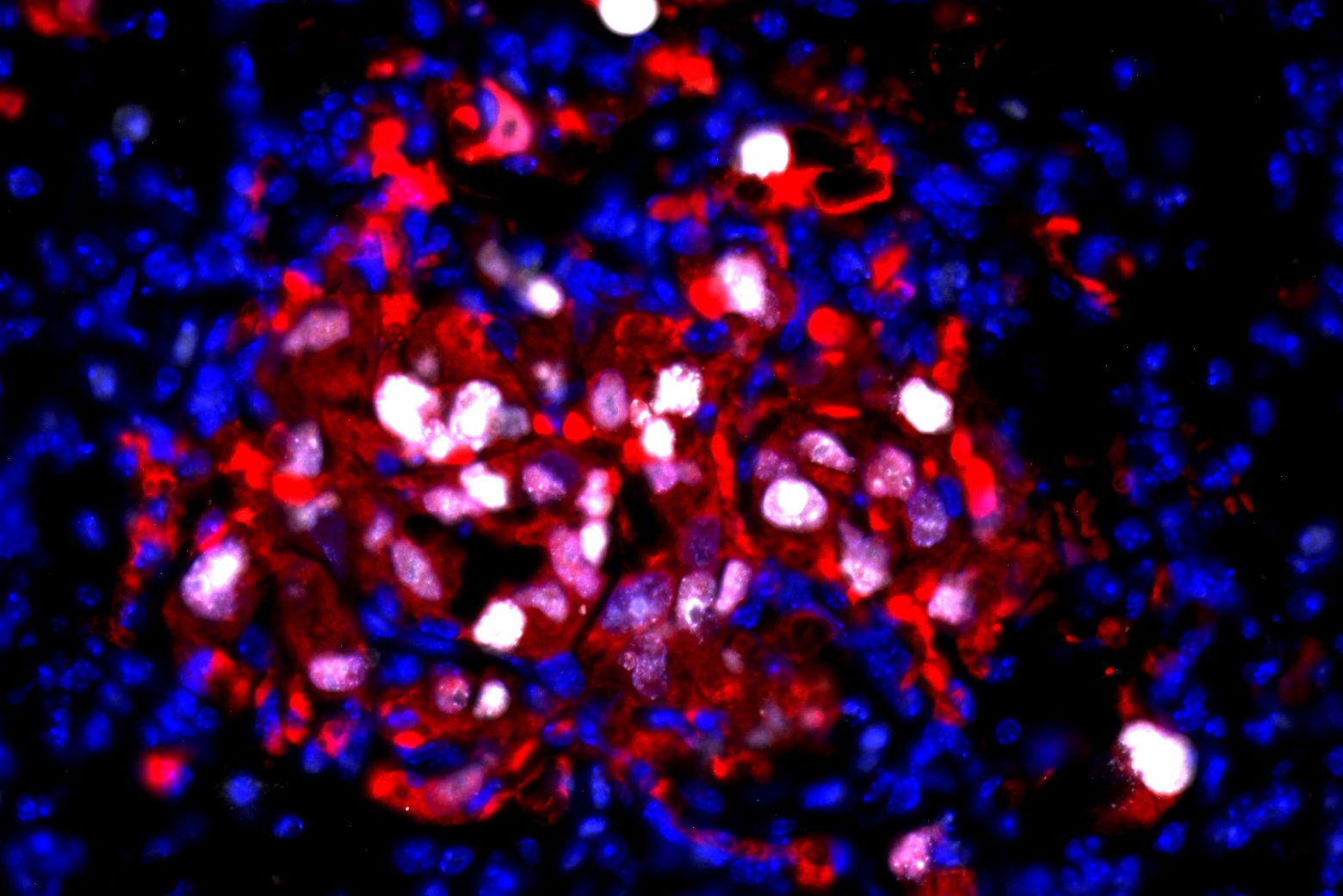
To investigate what makes this dormancy reversible months or years down the line, researchers in the Weinberg Lab injected human breast cancer cells into mice. These cancer cells were modified to produce a fluorescent protein, allowing the scientists to track their behavior in the body.
The group then focused on cancer cells that had lodged themselves in the lung tissue. By examining them for specific proteins—Ki67, ITGB4 and p63—that act as markers of cell activity and state, the researchers were able to confirm that these cells were in a non-dividing, dormant state.
Previous work from the Weinberg Lab had shown that inflammation in organ tissue can provoke dormant breast cancer cells to start growing again. In this study, the team tested bleomycin—a chemotherapy drug known to cause lung inflammation—that can be given to patients after surgery to lower the risk of cancer recurrence.
The researchers found that lung inflammation from bleomycin was sufficient to trigger the growth of large lung cancer colonies in treated mice—and to shift the character of these once dormant cells to those that are more invasive and mobile.
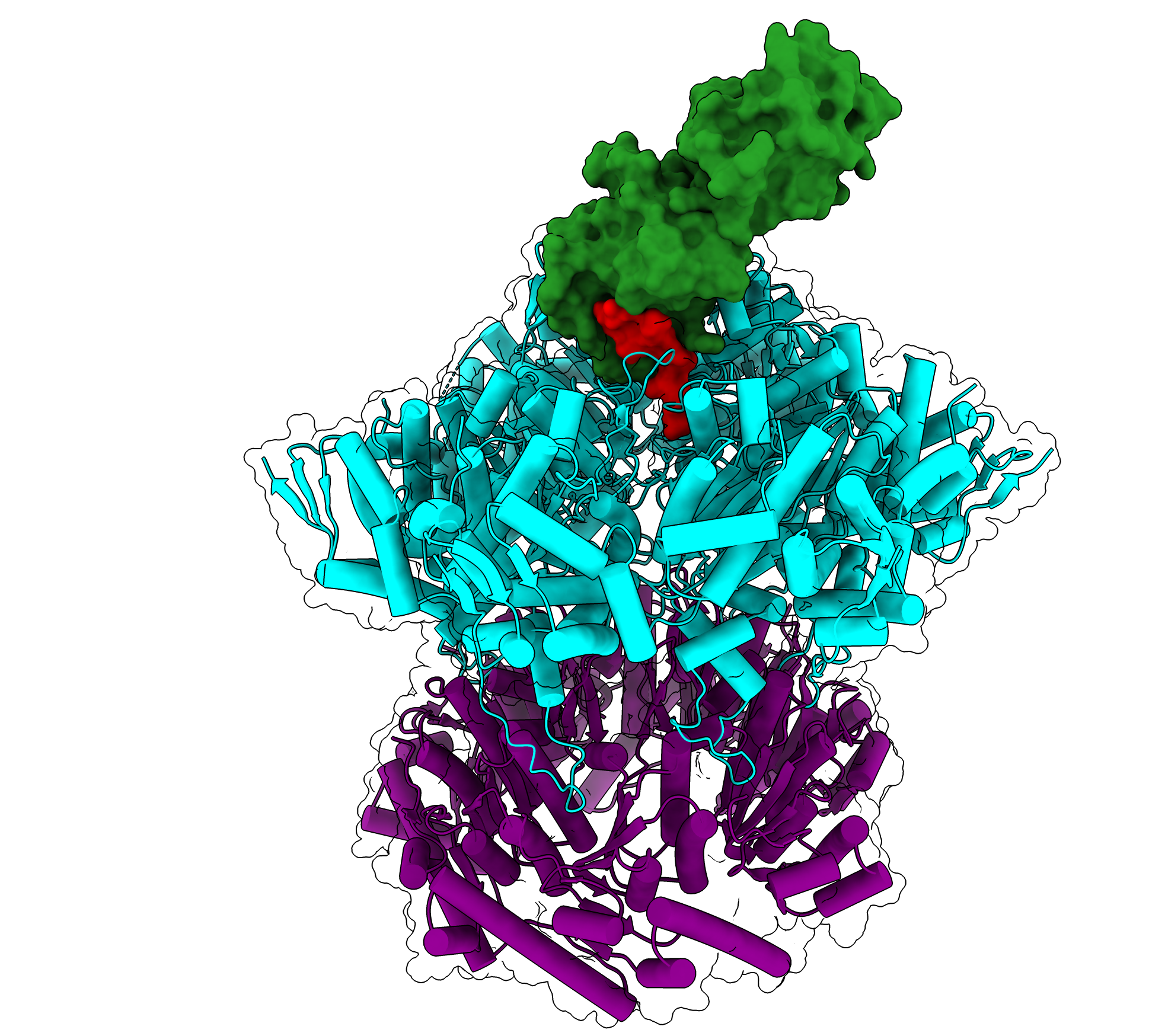
Zeroing in on the tumor microenvironment, the team identified a type of immune cells, called M2 macrophages, as drivers of this process. These macrophages release molecules called epidermal growth factor receptor (EGFR) ligands, which bind to receptors on the surface of dormant cancer cells. This activates a cascade of signals that provoke dormant cancer cells to start multiplying rapidly.
But EGFR signaling is only the initial spark that ignites the fire. “We found that once dormant cancer cells are awakened, they retain what we call an ‘awakening memory,’” Zhang says. “They no longer require ongoing inflammatory signals from the microenvironment to stay active [growing and multiplying]—they remember the awakened state.”
While signals related to inflammation are necessary to awaken dormant cancer cells, exactly how much signaling is needed remains unclear. “This aspect of cancer biology is particularly challenging because multiple signals contribute to the state change in these dormant cells,” Zhang says.
The team has already identified one key player in the awakening process but understanding the full set of signals and how each contributes is far more complex—a question they are continuing to investigate in their new work.
Studying these pivotal changes in the lives of cancer cells—such as their transition from dormancy to active growth—will deepen our scientific understanding of metastasis and, as researchers in the Weinberg Lab hope, lead to more effective treatments for patients with metastatic cancers.