The KATMAP model, developed by researchers in the Department of Biology, can predict alternative cell splicing, which allows cells to create endless diversity from the same sets of genetic blueprints.
Lillian Eden | Department of Biology
November 4, 2025
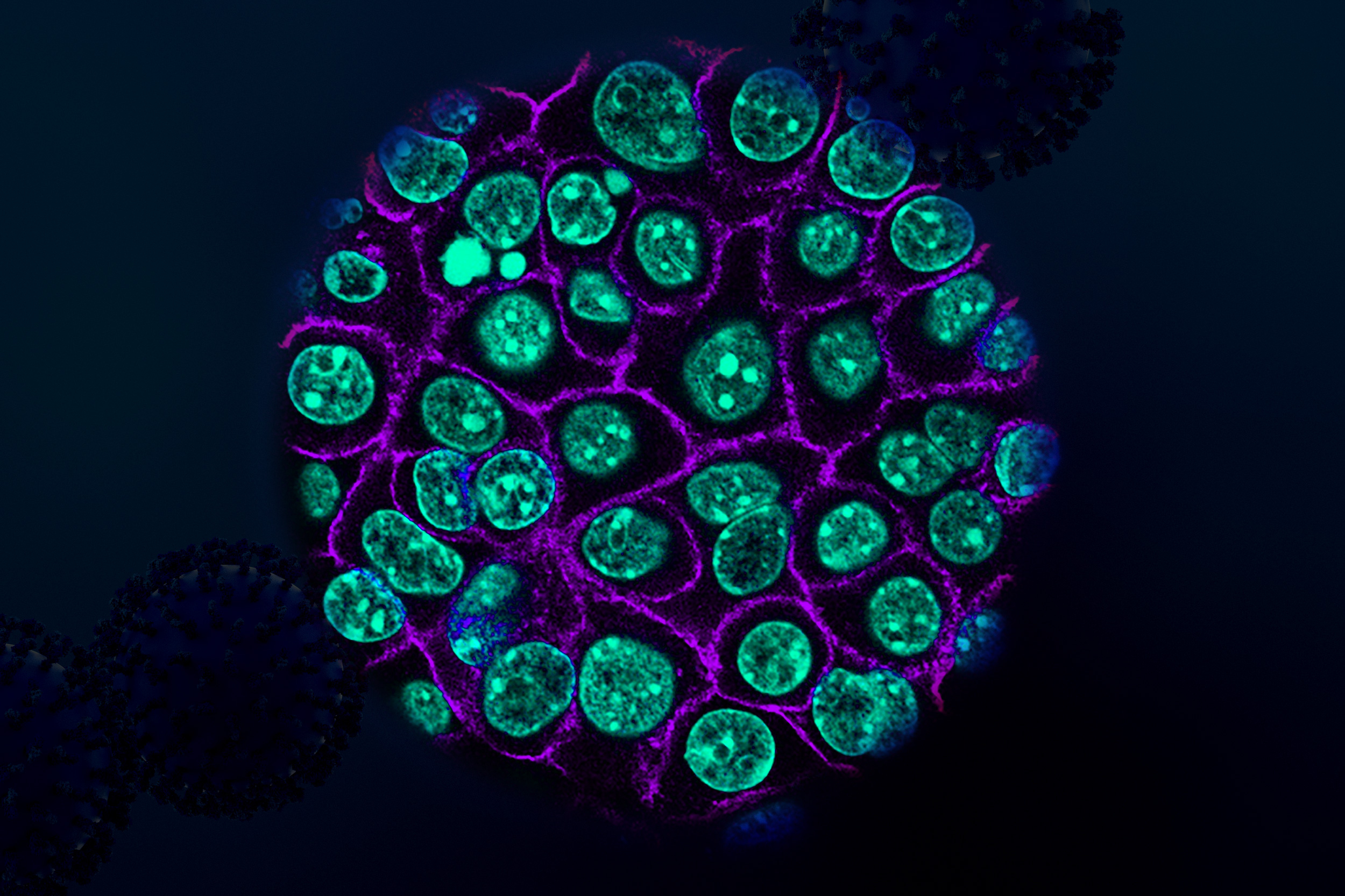
Although heart cells and skin cells contain identical instructions for creating proteins encoded in their DNA, they’re able to fill such disparate niches because molecular machinery can cut out and stitch together different segments of those instructions to create endlessly unique combinations.
The ingenuity of using the same genes in different ways is made possible by a process called splicing and is controlled by splicing factors; which splicing factors a cell employs determines what sets of instructions that cell produces, which, in turn, gives rise to proteins that allow cells to fulfill different functions.
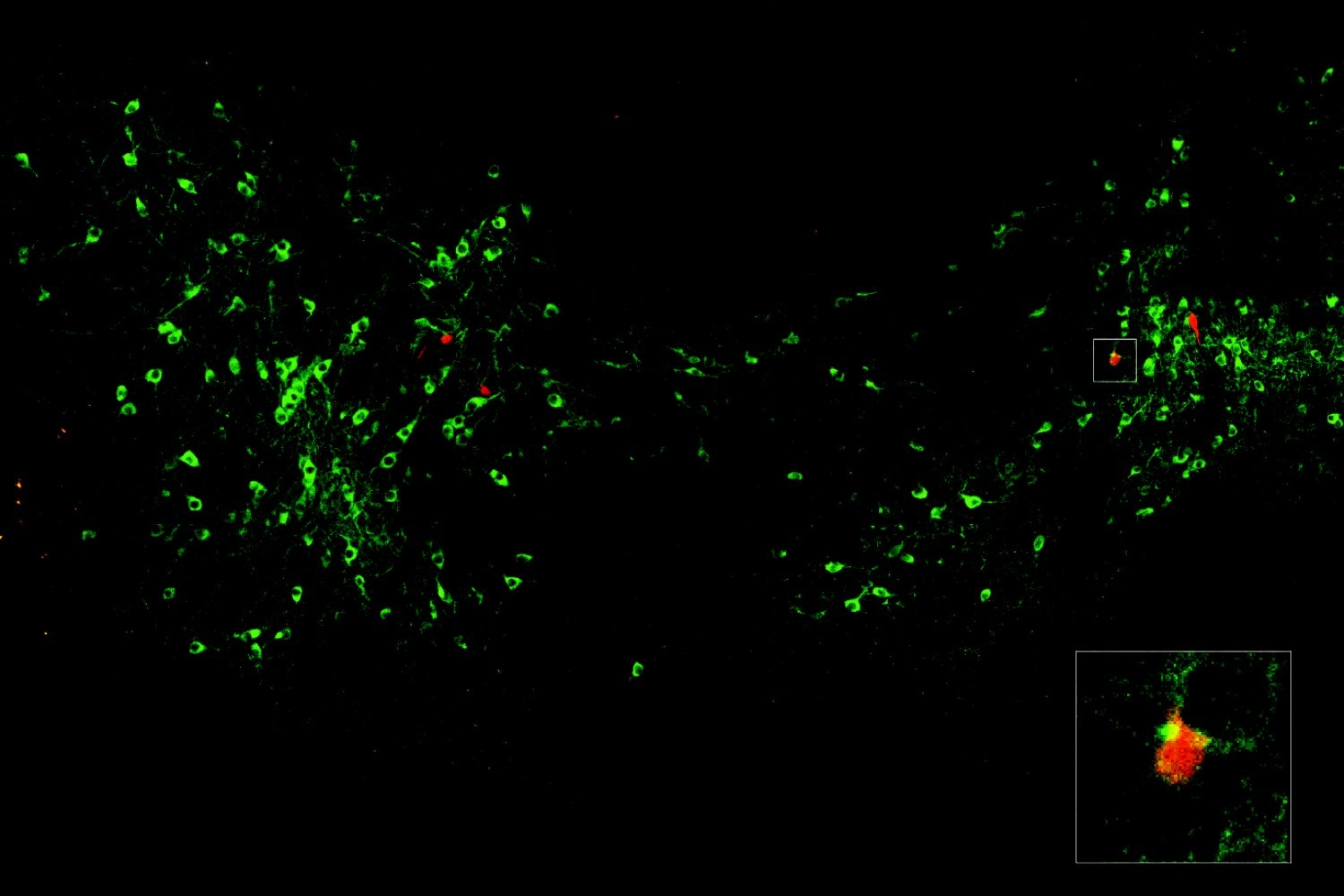
In an open-access paper published today in Nature Biotechnology, researchers in the MIT Department of Biology outlined a framework for parsing the complex relationship between sequences and splicing regulation to investigate the regulatory activities of splicing factors, creating models that can be applied to interpret and predict splicing regulation across different cell types, and even different species. Called Knockdown Activity and Target Models from Additive regression Predictions, KATMAP draws on experimental data from disrupting the expression of a splicing factor and information on which sequences the splicing factor interacts with to predict its likely targets.
Aside from the benefits of a better understanding of gene regulation, splicing mutations — either in the gene that is spliced or in the splicing factor itself — can give rise to diseases such as cancer by altering how genes are expressed, leading to the creation or accumulation of faulty or mutated proteins. This information is critical for developing therapeutic treatments for those diseases. The researchers also demonstrated that KATMAP can potentially be used to predict whether synthetic nucleic acids, a promising treatment option for disorders including a subset of muscular atrophy and epilepsy disorders, affect splicing.
Perturbing splicing
In eukaryotic cells, including our own, splicing occurs after DNA is transcribed to produce an RNA copy of a gene, which contains both coding and non-coding regions of RNA. The noncoding intron regions are removed, and the coding exon segments are spliced back together to make a near-final blueprint, which can then be translated into a protein.
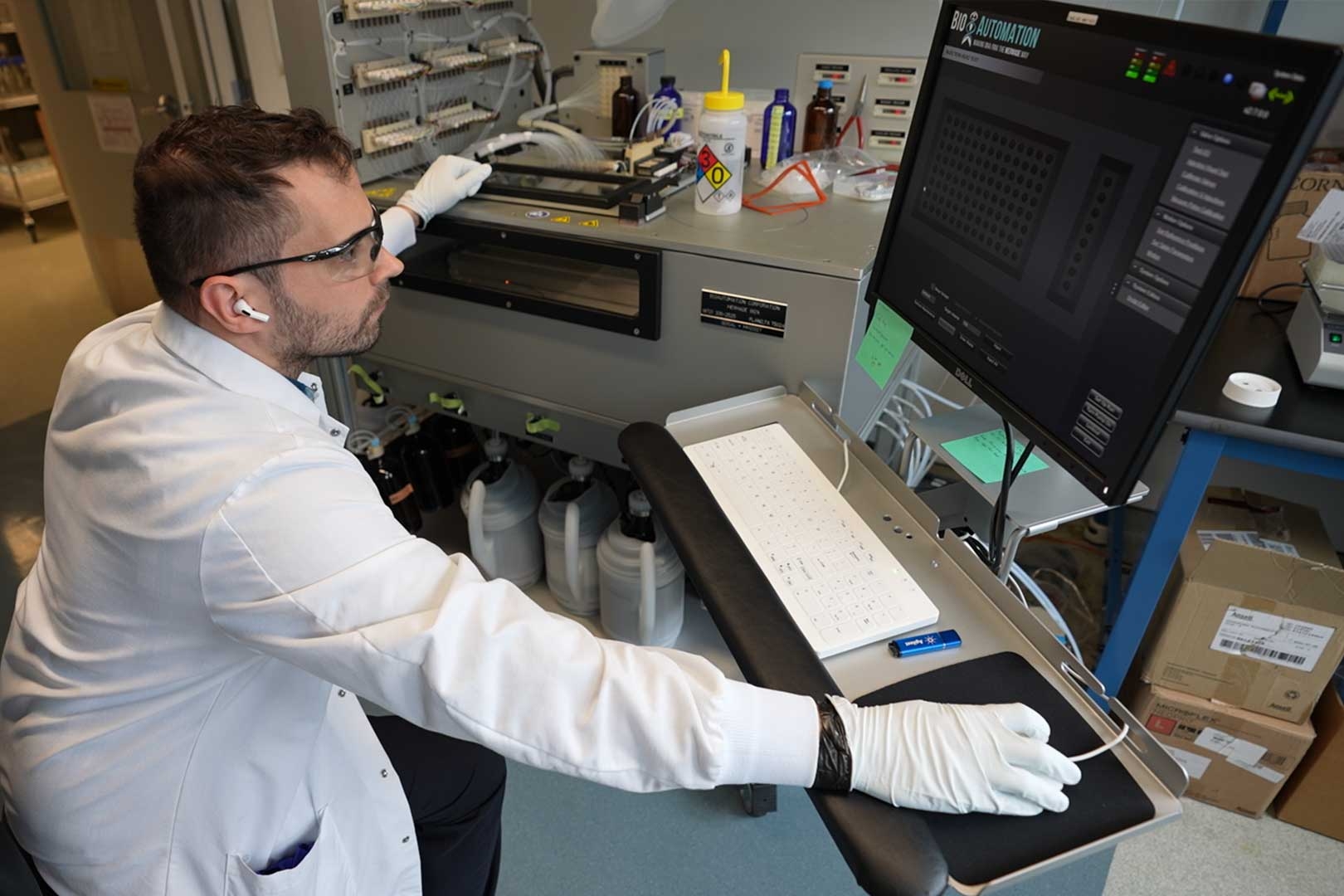
According to first author Michael P. McGurk, a postdoc in the lab of MIT Professor Christopher Burge, previous approaches could provide an average picture of regulation, but could not necessarily predict the regulation of splicing factors at particular exons in particular genes.
KATMAP draws on RNA sequencing data generated from perturbation experiments, which alter the expression level of a regulatory factor by either overexpressing it or knocking down its levels. The consequences of overexpression or knockdown are that the genes regulated by the splicing factor should exhibit different levels of splicing after perturbation, which helps the model identify the splicing factor’s targets.
Cells, however, are complex, interconnected systems, where one small change can cause a cascade of effects. KATMAP is also able to distinguish between direct targets from indirect, downstream impacts by incorporating known information about the sequence the splicing factor is likely to interact with, referred to as a binding site or binding motif.
“In our analyses, we identify predicted targets as exons that have binding sites for this particular factor in the regions where this model thinks they need to be to impact regulation,” McGurk says, while non-targets may be affected by perturbation but don’t have the likely appropriate binding sites nearby.
This is especially helpful for splicing factors that aren’t as well-studied.
“One of our goals with KATMAP was to try to make the model general enough that it can learn what it needs to assume for particular factors, like how similar the binding site has to be to the known motif or how regulatory activity changes with the distance of the binding sites from the splice sites,” McGurk says.
Starting simple
Although predictive models can be very powerful at presenting possible hypotheses, many are considered “black boxes,” meaning the rationale that gives rise to their conclusions is unclear. KATMAP, on the other hand, is an interpretable model that enables researchers to quickly generate hypotheses and interpret splicing patterns in terms of regulatory factors while also understanding how the predictions were made.
“I don’t just want to predict things, I want to explain and understand,” McGurk says. “We set up the model to learn from existing information about splicing and binding, which gives us biologically interpretable parameters.”
The researchers did have to make some simplifying assumptions in order to develop the model. KATMAP considers only one splicing factor at a time, although it is possible for splicing factors to work in concert with one another. The RNA target sequence could also be folded in such a way that the factor wouldn’t be able to access a predicted binding site, so the site is present but not utilized.
“When you try to build up complete pictures of complex phenomena, it’s usually best to start simple,” McGurk says. “A model that only considers one splicing factor at a time is a good starting point.”
David McWaters, another postdoc in the Burge Lab and a co-author on the paper, conducted key experiments to test and validate that aspect of the KATMAP model.
Future directions
The Burge lab is collaborating with researchers at Dana-Farber Cancer Institute to apply KATMAP to the question of how splicing factors are altered in disease contexts, as well as with other researchers at MIT as part of an MIT HEALS grant to model splicing factor changes in stress responses. McGurk also hopes to extend the model to incorporate cooperative regulation for splicing factors that work together.
“We’re still in a very exploratory phase, but I would like to be able to apply these models to try to understand splicing regulation in disease or development. In terms of variation of splicing factors, they are related, and we need to understand both,” McGurk says.
Burge, the Uncas (1923) and Helen Whitaker Professor and senior author of the paper, will continue to work on generalizing this approach to build interpretable models for other aspects of gene regulation.
“We now have a tool that can learn the pattern of activity of a splicing factor from types of data that can be readily generated for any factor of interest,” says Burge, who is also an extra-mural member of the Koch Institute for Integrative Cancer Research and an associate member of the Broad Institute of MIT and Harvard. “As we build up more of these models, we’ll be better able to infer which splicing factors have altered activity in a disease state from transcriptomic data, to help understand which splicing factors are driving pathology.”