By researching the effects of sex chromosomes on two types of immune cells, researchers in the Page Lab explore the biological underpinnings of sex biases in immunity and autoimmune disease
Greta Friar | Whitehead Institute
August 6, 2024
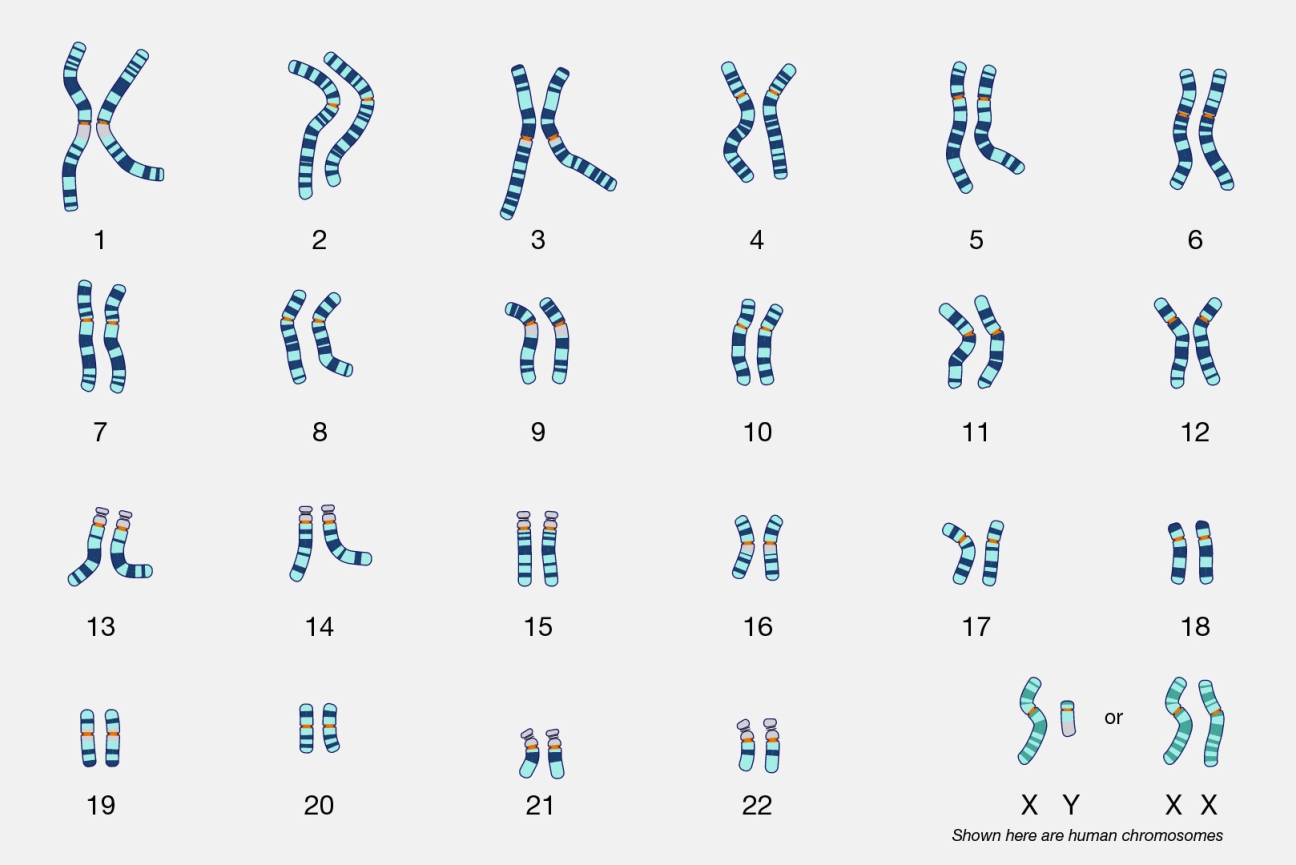
There are many known sex differences in health and disease: cases in which either men or women are more likely to get a disease, experience a symptom, or have a certain drug side effect. Some of these sex differences are caused by social and environmental factors: for example, when men smoked more than women, men were more likely to develop lung cancer. However, some have biological underpinnings. For example, men are more likely to be red-green colorblind because the relevant gene is on the X chromosome, of which men with XY chromosomes have no backup copy for a dysfunctional version.
Often, the specific factors contributing to a sex difference are hard to tease apart; there may not be a simple way to tell what is caused by sex chromosomes versus sex hormones versus environment. To address this question, researchers in Whitehead Institute Member David Page’s lab previously developed an approach to identify the contributions of the sex chromosomes to sex differences. Now, Page and former postdoc in his lab Laura Blanton have built on that work by measuring the effects of the sex chromosomes on two types of immune cells. The work, published in the journal Cell Genomics on August 6, shows that sex chromosome gene expression is consistent across cell types, but that its effects are cell type specific.
Sex differences are common in the function and dysfunction of our immune system. Examples include the typically weaker male immune response to pathogens and vaccines, and the female-biased frequency of autoimmune diseases. Page and Blanton’s work in immune cells examines several genes that have been implicated in such sex differences.
Developing a method to measure sex chromosome influence
The approach that the researchers used is based on several facts about sex chromosomes. Firstly, although females typically have two X chromosomes and males typically have one X and one Y, there are people with rare combinations of sex chromosomes, who have anywhere from 1-5 X chromosomes and 0-4 Y chromosomes. Secondly, there are two types of X chromosome: The active X chromosome (Xa) and the inactive X chromosome (Xi). They are genetically identical, but many of the genes on Xi are either switched off or have their expression level dialed way down.
Xa does not really function as a sex chromosome since everyone in the world has exactly one Xa regardless of their sex. In people with more than one X chromosome, any additional X chromosomes are always Xi. Furthermore, Page and Blanton’s research demonstrates that Xa responds to gene expression by Xi and Y—the sex chromosomes—in the same manner as do the other 22 pairs of non-sex chromosomes—the autosomes.
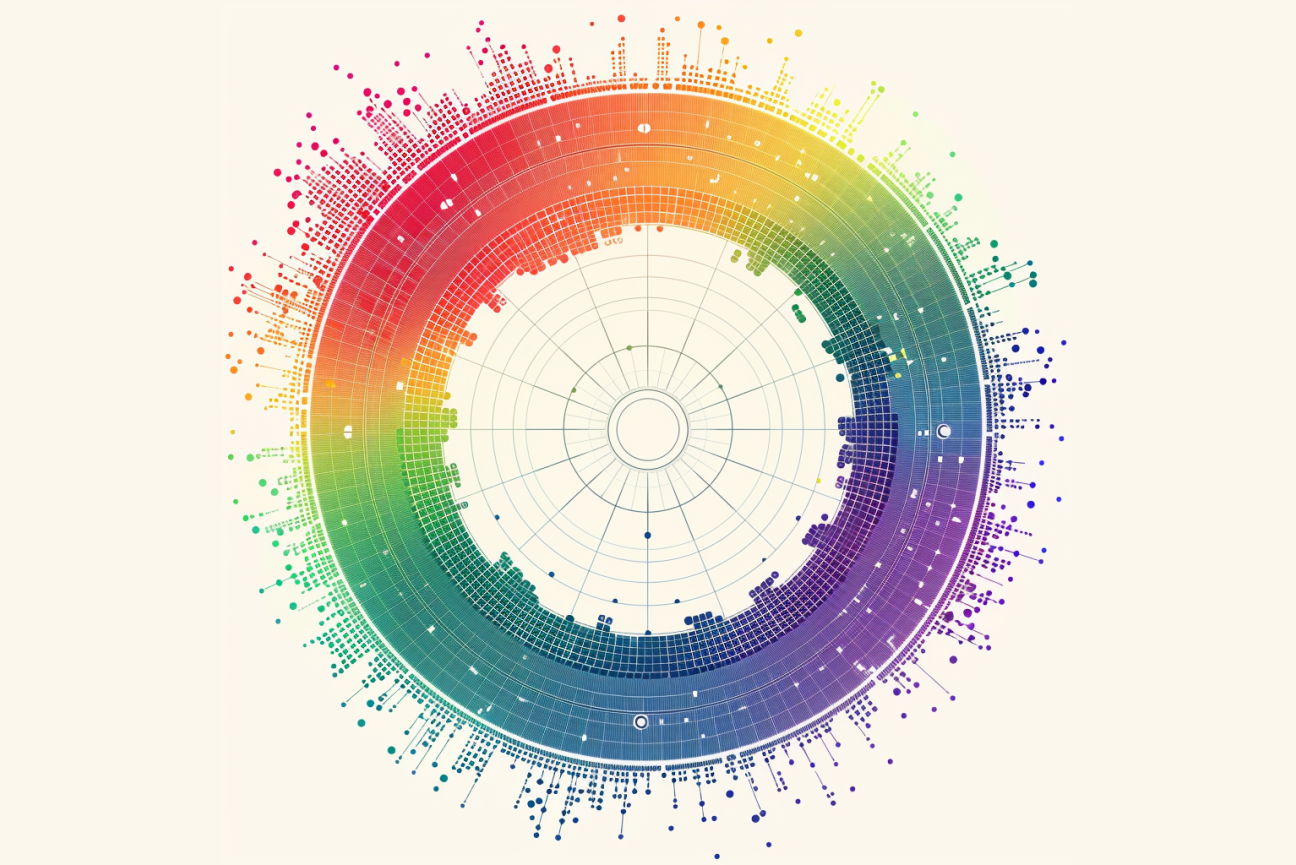
With these facts in mind, the researchers collected cells from donors with different combinations of sex chromosomes. Then they measured the expression of every gene in these cells, across the donor population, and observed how the expression of each gene changed with the addition of each Xi or Y chromosome.
This approach was first shared in a Cell Genomics paper by Page and former postdoc Adrianna San Roman in 2023. They had cultured two types of cells, fibroblasts and lymphoblastoid cell lines, from donor tissue samples. They found that the effects of Xi and Y were modular—each additional chromosome changed gene expression by about the same amount. This approach allowed the researchers to identify which genes are sensitive to regulation by the sex chromosomes, and to measure the strength of the effect for each responsive gene.
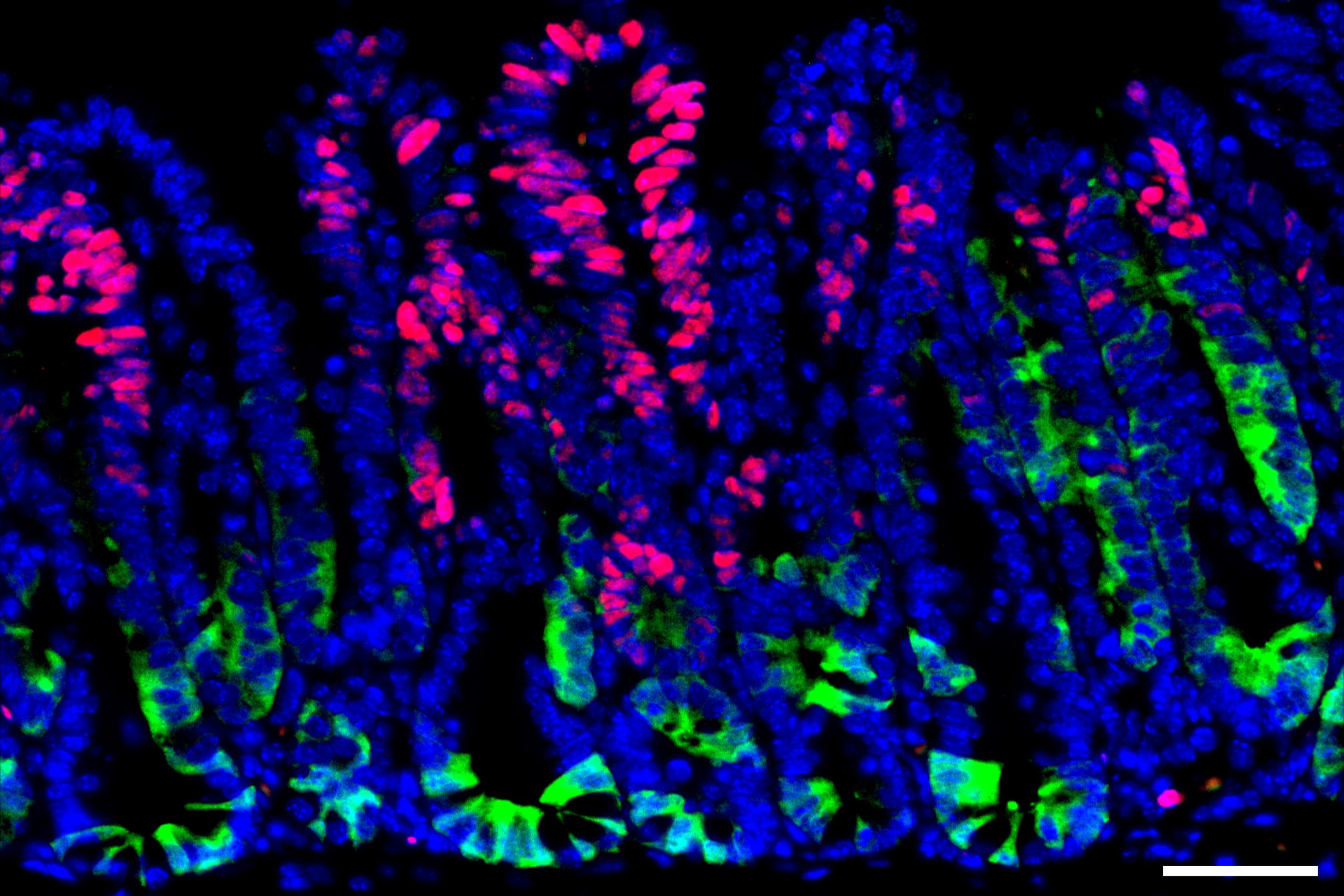
In that and a following paper, Page and San Roman looked at how Xi and Y affect gene expression from Xa and the autosomes. Blanton expanded the study of Xi and Y by using the same approach in two types of immune cells, monocytes and CD4+ T cells, taken directly from donors’ blood. Studying cells taken directly from the body, rather than cells cultured in the lab, enabled the researchers to confirm that their observations applied in both conditions.
In all three papers, the researchers found that the sex chromosomes have significant effects on the expression levels of many genes that are active throughout the body. They also identified a particular pair of genes as driving much of this effect in all four cell types. The genes, ZFX and ZFY, found on the X and Y chromosomes respectively, are transcription factors that can dial up the expression of other genes. The pair originates from the same ancestral gene, and although they have grown slightly apart since the X and Y chromosomes diverged, they still perform the same gene regulatory function. The researchers found that they tended to affect expression of the same gene targets by similar though not identical amounts.
In other words, the presence of either sex chromosome causes roughly the same effect on expression of autosomal and Xa genes. This similarity makes sense: carefully calibrated gene regulation is necessary in every body, and so each sex chromosome must maintain that function. It does, however, make it harder to spot the cases in which sex chromosomes contribute to sex differences in health and disease.
“Sex differences in health and disease could stem from the rare instances in which one gene responds very differently to Xi versus Y—we found cases where that occurs,” Blanton says. “They could also stem from subtle differences in the gene expression changes caused by Xi and Y that build up into larger effects downstream.”
Blanton then combined her and San Roman’s data in order to look at how the effects of sex chromosome dosage—how many Xs or Ys are in a cell—compared across all four cell types.
The effects of sex chromosomes on immune cells
Blanton found that gene expression from the sex chromosomes was consistent across all four cell types. The exceptions to this rule were always X chromosome genes that are only expressed on Xa, and so could be regulated by Xi and Y in the way that autosomal genes are. This contrasts with speculation that different genes on Xi might be silenced in different cells.
However, each cell type had a distinct response to this identical sex chromosome gene expression. Different biological pathways were affected, or the same biological pathway could be affected in the opposite direction. Key immune cell processes affected by sex chromosome dosage in either monocytes or T cells included production of immune system proteins, signaling, and inflammatory response.
The cell type specific responses were due to different genes responding to the sex chromosomes in each cell type. The researchers do not yet know the mechanism causing the same gene to respond to sex chromosome dosage in one cell type but not another. One possibility is that access to the genes is blocked in some of the cell types. Regions of DNA can become tightly packed so that a gene, or a DNA region that regulates the gene, becomes inaccessible to transcription factors such as ZFX and ZFY, and so they cannot affect the gene’s expression. Another possibility is that the genes might require specific partner molecules in order for their expression level to increase, and that these partners may be present in one cell type but not the other.
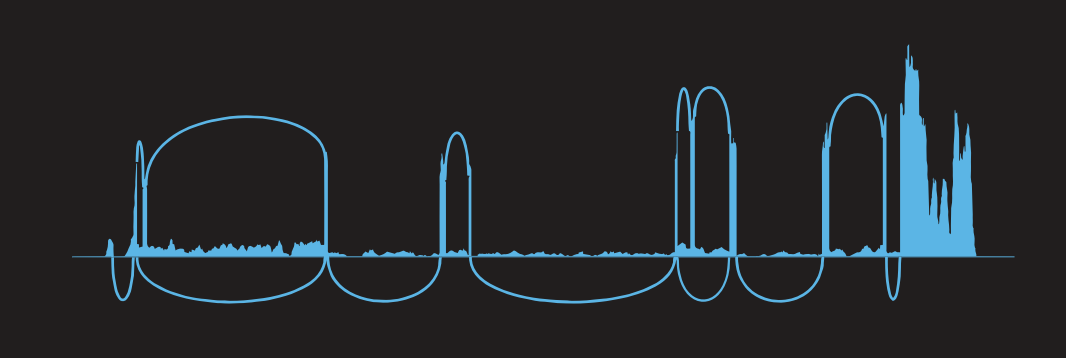
Blanton also measured how X chromosome dosage affected T cells in their inactive state, when there is no perceived immune threat, versus their activated state, when they begin to produce an immune response and replicate themselves. Increases in X chromosome dosage led to heightened activation, with increased expression of genes related to proliferation. This finding highlights the importance of looking at how sex chromosomes affect not just different cell types, but cells in different states or scenarios.
“As we learn what pathways the sex chromosomes influence in each cell type, we can begin to make sense of the contributions of the sex chromosomes to each cell type’s functions and its roles in disease,” Blanton says.
Although Page and Blanton found that the presence of an Xi or Y chromosome had very similar effects on most genes, the researchers did identify one interesting case in which response to X and Y differed. FCG2RB is a gene involved in immunity that has been implicated in and thought to contribute to the female bias in developing systemic lupus erythematosus (SLE). Blanton found that unlike most genes, FCGR2B is sensitive to X and not Y chromosome dosage. This strengthens the case that higher expression of FCGR2B could be driving the SLE female bias.
“FCGR2B provides a promising opportunity to study the contributions of the sex chromosomes to a sex bias in disease, and to learn more about the biology of a chronic disease that affects many people around the world,” Page says.
In other cases, the researchers found that genes which have been suspected to contribute to female bias in disease did not have a strong response to X chromosome dosage. For example, TLR7 is thought to contribute to female bias in developing autoimmunity, and CD40LG is thought to contribute to female bias in developing lupus. Neither of the genes showed increased expression as X chromosome dosage increased. This suggests that other mechanisms may be driving the sex bias in these cases.
Because of the limited pool of donors, the researchers were not able to identify every gene that responds to sex chromosome dosage, and future research may uncover more sex-chromosome-sensitive genes of interest. Meanwhile, the Page lab continues to investigate the sex chromosomes’ shared role as regulators of gene expression throughout the body.
“We’ve got to recalibrate our thinking from the view that X and Y are mainly involved in differentiating males and females, to understanding that they also have largely shared functions that are important throughout the body,” Page says. “At the same time, I think that uncovering the biology of Xi is going to be incredibly important for understanding women’s health and sex differences in health and disease.”