Differences in male and female gene expression, including those contributing to height differences, found throughout the body in humans and other mammals.
Greta Friar | Whitehead Institute
July 19, 2019
Throughout the animal kingdom, males and females frequently exhibit sexual dimorphism: differences in characteristic traits that often make it easy to tell them apart. In mammals, one of the most common sex-biased traits is size, with males typically being larger than females. This is true in humans: Men are, on average, taller than women. However, biological differences among males and females aren’t limited to physical traits like height. They’re also common in disease. For example, women are much more likely to develop autoimmune diseases, while men are more likely to develop cardiovascular diseases.
In spite of the widespread nature of these sex biases, and their significant implications for medical research and treatment, little is known about the underlying biology that causes sex differences in characteristic traits or disease. In order to address this gap in understanding, Whitehead Institute Director David Page has transformed the focus of his lab in recent years from studying the X and Y sex chromosomes to working to understand the broader biology of sex differences throughout the body. In a paper published in Science, Page, a professor of biology at MIT and a Howard Hughes Medical Institute investigator; Sahin Naqvi, first author and former MIT graduate student (now a postdoc at Stanford University); and colleagues present the results of a wide-ranging investigation into sex biases in gene expression, revealing differences in the levels at which particular genes are expressed in males versus females.
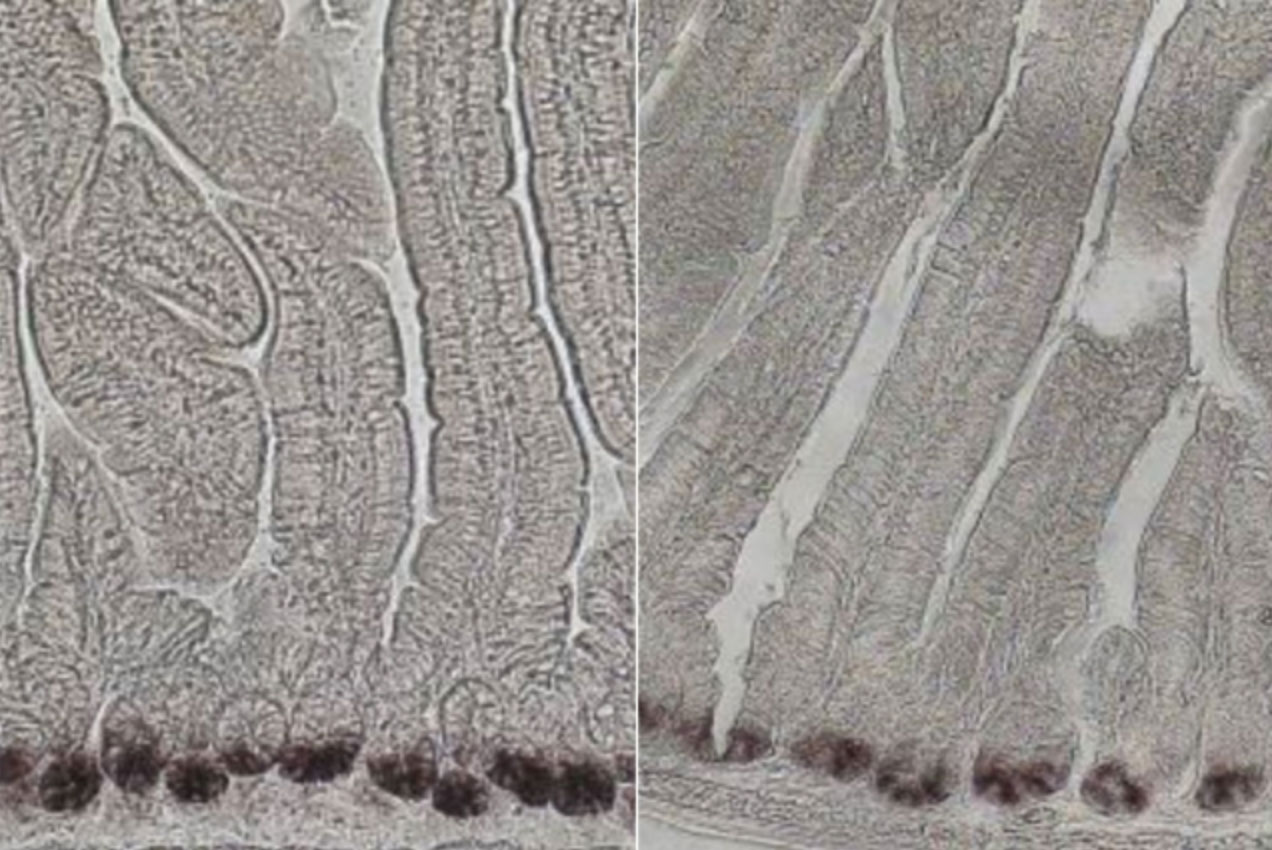
The researchers’ findings span 12 tissue types in five species of mammals, including humans, and led to the discovery that a combination of sex-biased genes accounts for approximately 12 percent of the average height difference between men and women. This finding demonstrates a functional role for sex-biased gene expression in contributing to sex differences. The researchers also found that the majority of sex biases in gene expression are not shared between mammalian species, suggesting that — in some cases — sex-biased gene expression that can contribute to disease may differ between humans and the animals used as models in medical research.
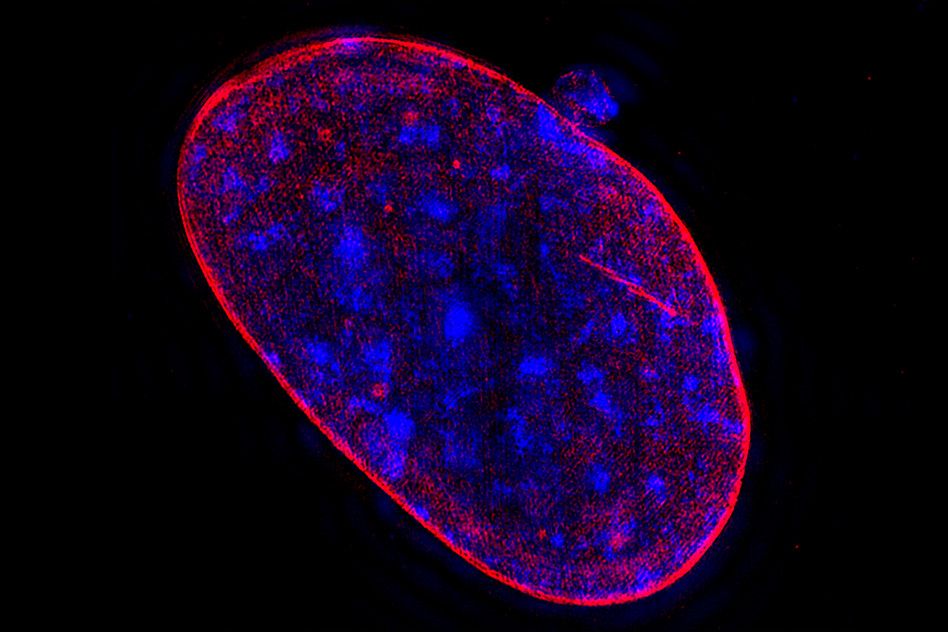
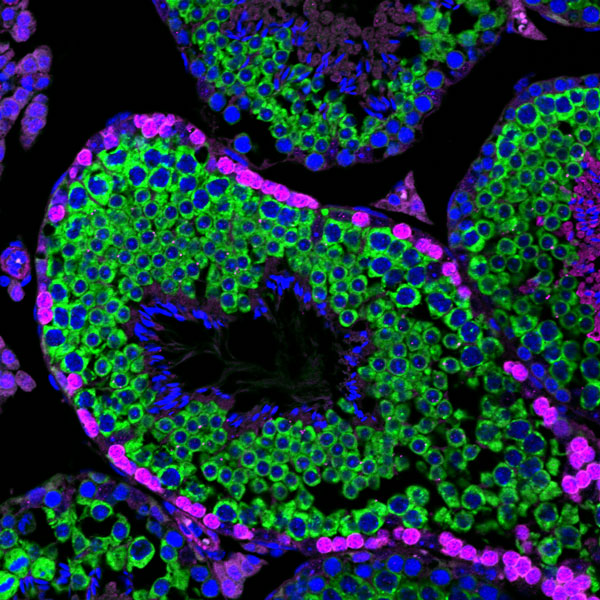
Having the same gene expressed at different levels in each sex is one way to perpetuate sex differences in traits in spite of the genetic similarity of males and females within a species — since with the exception of the 46th chromosome (the Y in males or the second X in females), the sexes share the same pool of genes. For example, if a tall parent passes on a gene associated with an increase in height to both a son and a daughter, but the gene has male-biased expression, then that gene will be more highly expressed in the son, and so may contribute more height to the son than the daughter.
The researchers searched for sex-biased genes in tissues across the body in humans, macaques, mice, rats, and dogs, and they found hundreds of examples in every tissue. They used height for their first demonstration of the contribution of sex-biased gene expression to sex differences in traits because height is an easy-to-measure and heavily studied trait in quantitative genetics.
“Discovering contributions of sex-biased gene expression to height is exciting because identifying the determinants of height is a classic, century-old problem, and yet by looking at sex differences in this new way we were able to provide new insights,” Page says. “My hope is that we and other researchers can repeat this model to similarly gain new insights into diseases that show sex bias.”
Because height is so well studied, the researchers had access to public data on the identity of hundreds of genes that affect height. Naqvi decided to see how many of those height genes appeared in the researchers’ new dataset of sex-biased genes, and whether the genes’ sex biases corresponded to the expected effects on height. He found that sex-biased gene expression contributed approximately 1.6 centimeters to the average height difference between men and women, or 12 percent of the overall observed difference.
The scope of the researchers’ findings goes beyond height, however. Their database contains thousands of sex-biased genes. Slightly less than a quarter of the sex-biased genes that they catalogued appear to have evolved that sex bias in an early mammalian ancestor, and to have maintained that sex bias today in at least four of the five species studied. The majority of the genes appear to have evolved their sex biases more recently, and are specific to either one species or a certain lineage, such as rodents or primates.
Whether or not a sex-biased gene is shared across species is a particularly important consideration for medical and pharmaceutical research using animal models. For example, previous research identified certain genetic variants that increase the risk of Type 2 diabetes specifically in women; however, the same variants increase the risk of Type 2 diabetes indiscriminately in male and female mice. Therefore, mice would not be a good model to study the genetic basis of this sex difference in humans. Even when the animal appears to have the same sex difference in disease as humans, the specific sex-biased genes involved might be different. Based on their finding that most sex bias is not shared between species, Page and colleagues urge researchers to use caution when picking an animal model to study sex differences at the level of gene expression.
“We’re not saying to avoid animal models in sex-differences research, only not to take for granted that the sex-biased gene expression behind a trait or disease observed in an animal will be the same as that in humans. Now that researchers have species and tissue-specific data available to them, we hope they will use it to inform their interpretation of results from animal models,” Naqvi says.
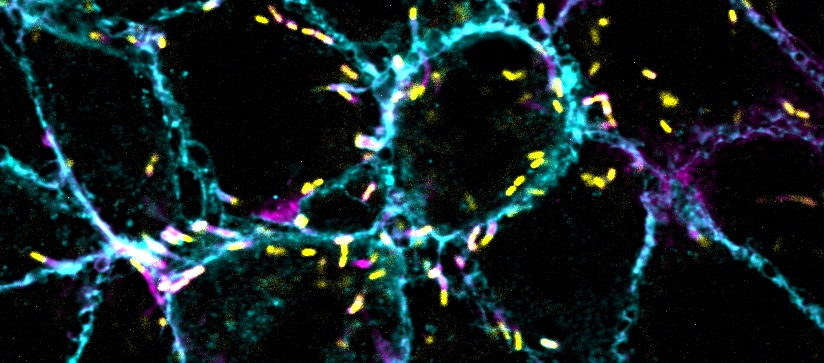
The researchers have also begun to explore what exactly causes sex-biased expression of genes not found on the sex chromosomes. Naqvi discovered a mechanism by which sex-biased expression may be enabled: through sex-biased transcription factors, proteins that help to regulate gene expression. Transcription factors bind to specific DNA sequences called motifs, and he found that certain sex-biased genes had the motif for a sex-biased transcription factor in their promoter regions, the sections of DNA that turn on gene expression. This means that, for example, a male-biased transcription factor was selectively binding to the promoter region for, and so increasing the expression of, male-biased genes — and likewise for female-biased transcription factors and female-biased genes. The question of what regulates the transcription factors remains for further study — but all sex differences are ultimately controlled by either the sex chromosomes or sex hormones.
The researchers see the collective findings of this paper as a foundation for future sex-differences research.
“We’re beginning to build the infrastructure for a systematic understanding of sex biases throughout the body,” Page says. “We hope these datasets are used for further research, and we hope this work gives people a greater appreciation of the need for, and value of, research into the molecular differences in male and female biology.”
This work was supported by Biogen, Whitehead Institute, National Institutes of Health, Howard Hughes Medical Institute, and generous gifts from Brit and Alexander d’Arbeloff and Arthur W. and Carol Tobin Brill.