The findings from the Yilmaz Lab recently published in Nature, may offer a new way to help heal tissue damage from radiation or chemotherapy treatment.
Anne Trafton | MIT News
October 1, 2025
A diet rich in the amino acid cysteine may have rejuvenating effects in the small intestine, according to a new study from MIT. This amino acid, the researchers discovered, can turn on an immune signaling pathway that helps stem cells to regrow new intestinal tissue.
This enhanced regeneration may help to heal injuries from radiation, which often occur in patients undergoing radiation therapy for cancer. The research was conducted in mice, but if future research shows similar results in humans, then delivering elevated quantities of cysteine, through diet or supplements, could offer a new strategy to help damaged tissue heal faster, the researchers say.
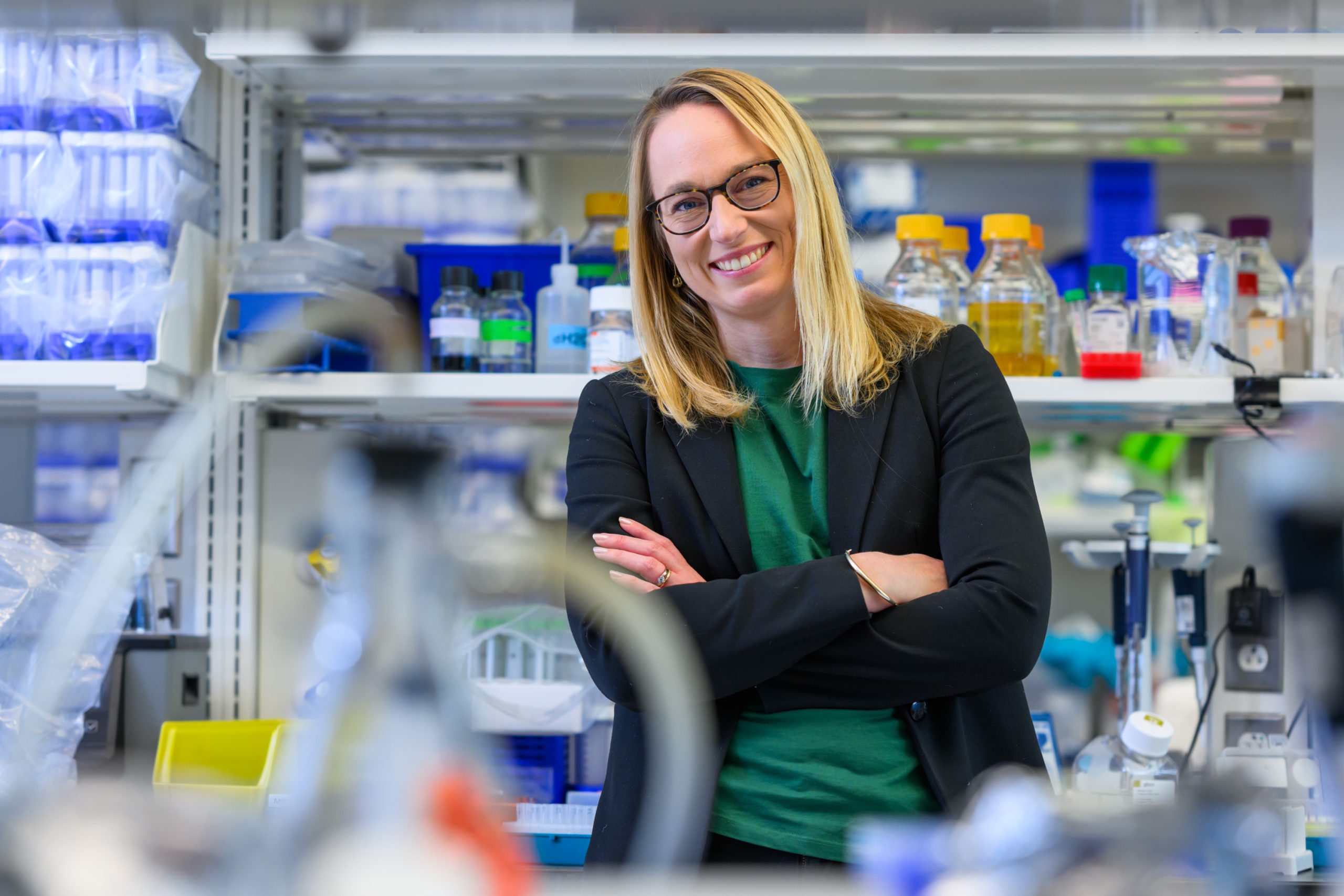
“The study suggests that if we give these patients a cysteine-rich diet or cysteine supplementation, perhaps we can dampen some of the chemotherapy or radiation-induced injury,” says Omer Yilmaz, director of the MIT Stem Cell Initiative, an associate professor of biology at MIT, and a member of MIT’s Koch Institute for Integrative Cancer Research. “The beauty here is we’re not using a synthetic molecule; we’re exploiting a natural dietary compound.”
While previous research has shown that certain types of diets, including low-calorie diets, can enhance intestinal stem cell activity, the new study is the first to identify a single nutrient that can help intestinal cells to regenerate.
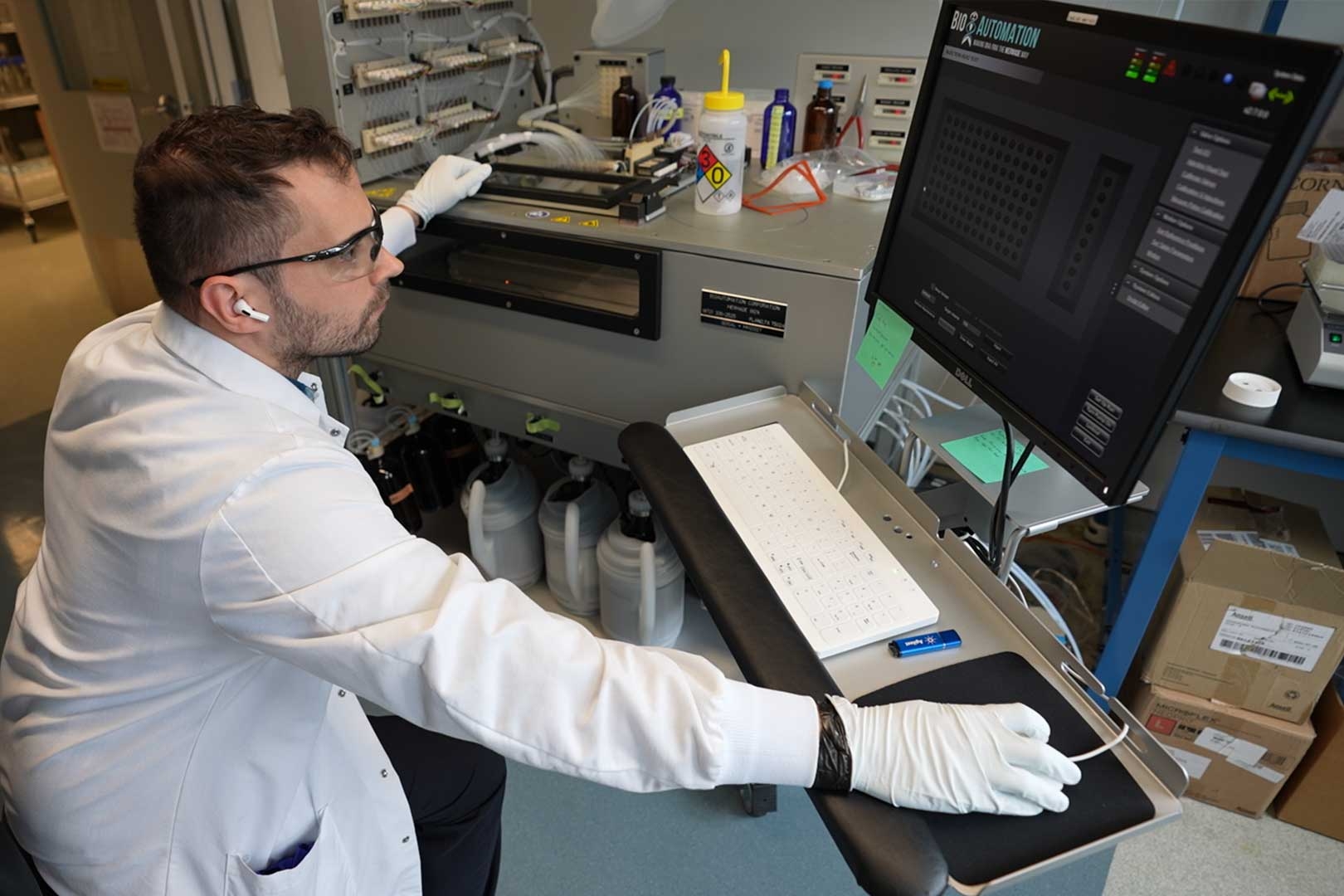
Yilmaz is the senior author of the study, which appears today in Nature. Koch Institute postdoc Fangtao Chi is the paper’s lead author.
Boosting regeneration
It is well-established that diet can affect overall health: High-fat diets can lead to obesity, diabetes, and other health problems, while low-calorie diets have been shown to extend lifespans in many species. In recent years, Yilmaz’s lab has investigated how different types of diets influence stem cell regeneration, and found that high-fat diets, as well as short periods of fasting, can enhance stem cell activity in different ways.
“We know that macro diets such as high-sugar diets, high-fat diets, and low-calorie diets have a clear impact on health. But at the granular level, we know much less about how individual nutrients impact stem cell fate decisions, as well as tissue function and overall tissue health,” Yilmaz says.
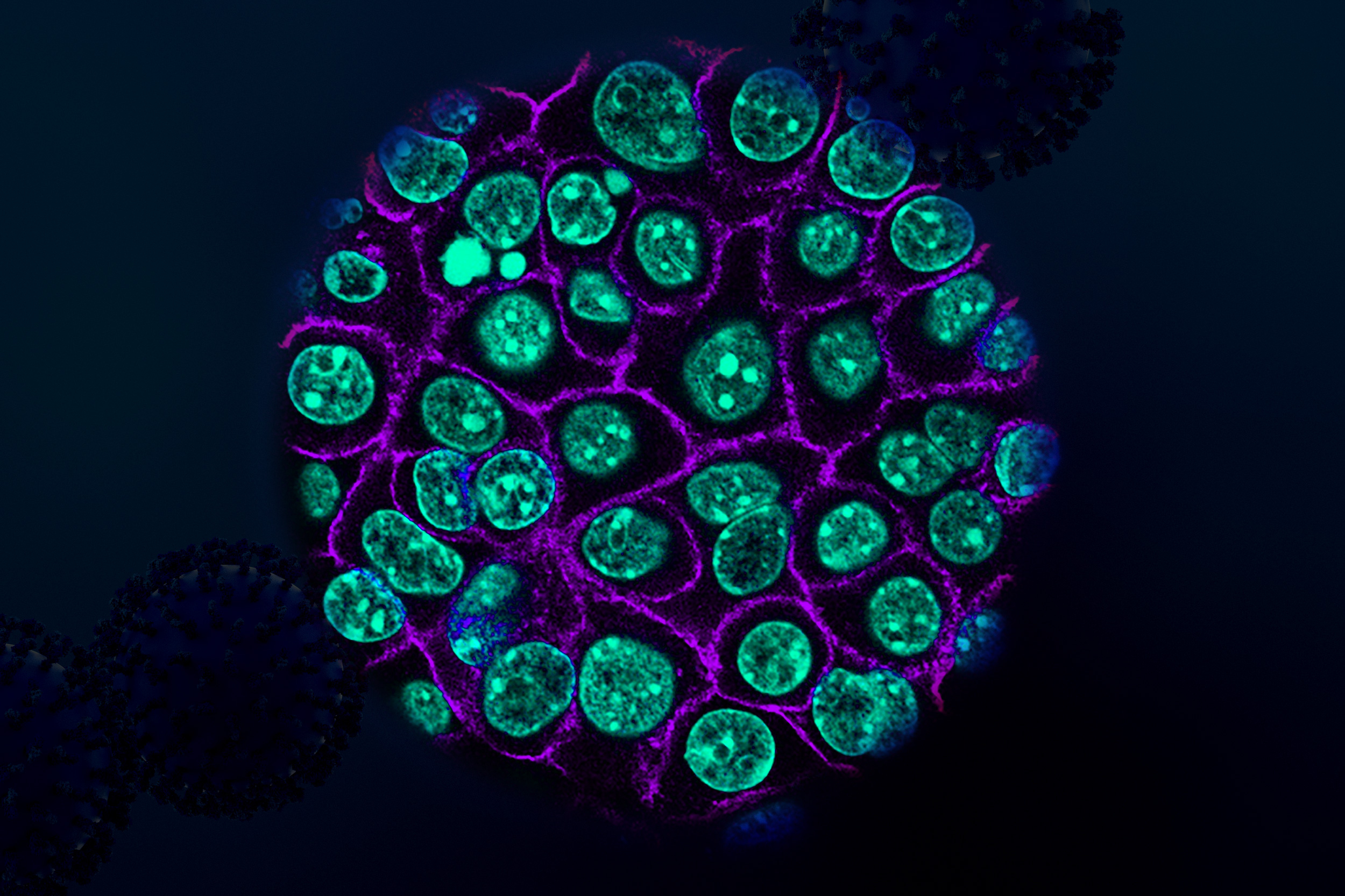
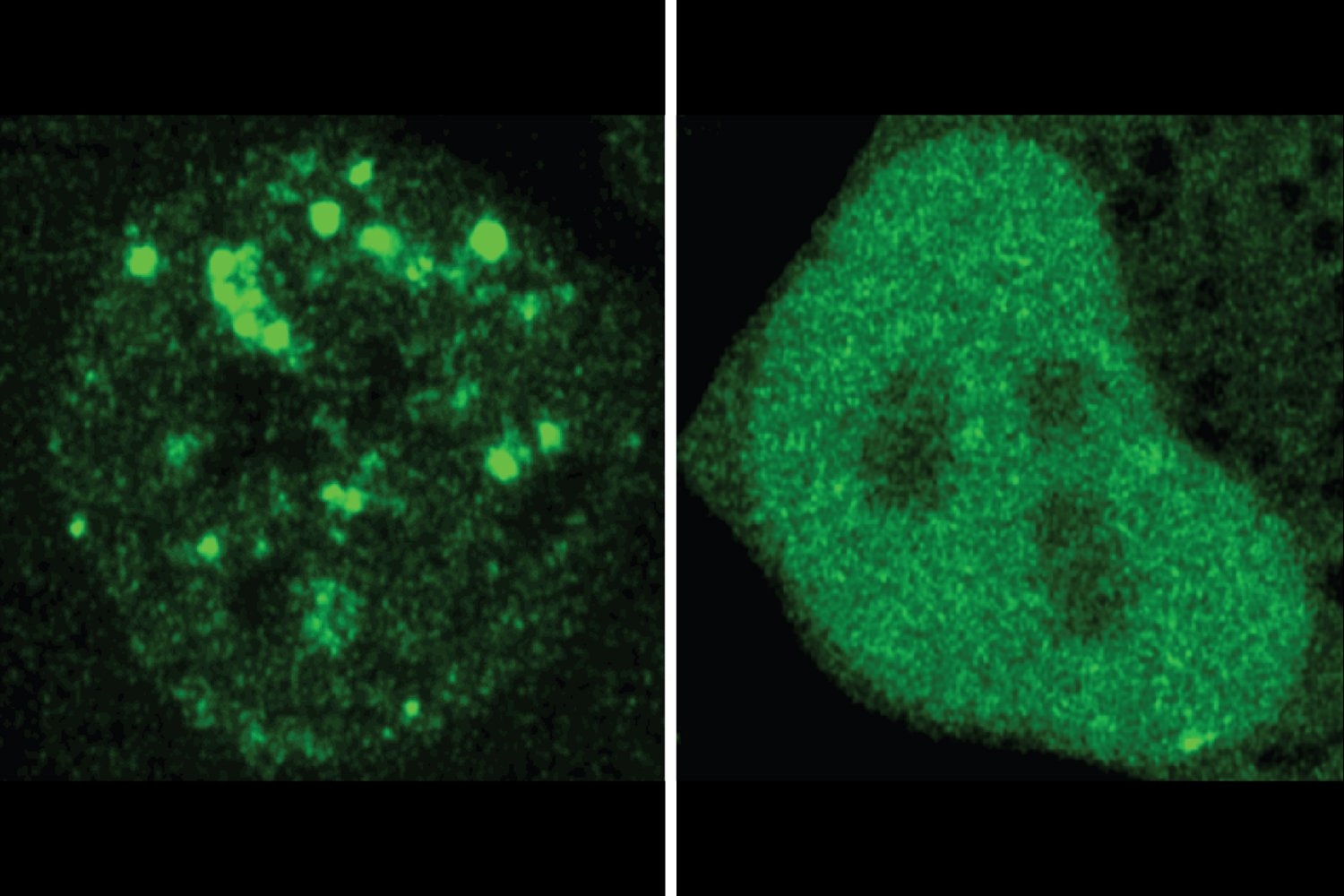
In their new study, the researchers began by feeding mice a diet high in one of 20 different amino acids, the building blocks of proteins. For each group, they measured how the diet affected intestinal stem cell regeneration. Among these amino acids, cysteine had the most dramatic effects on stem cells and progenitor cells (immature cells that differentiate into adult intestinal cells).
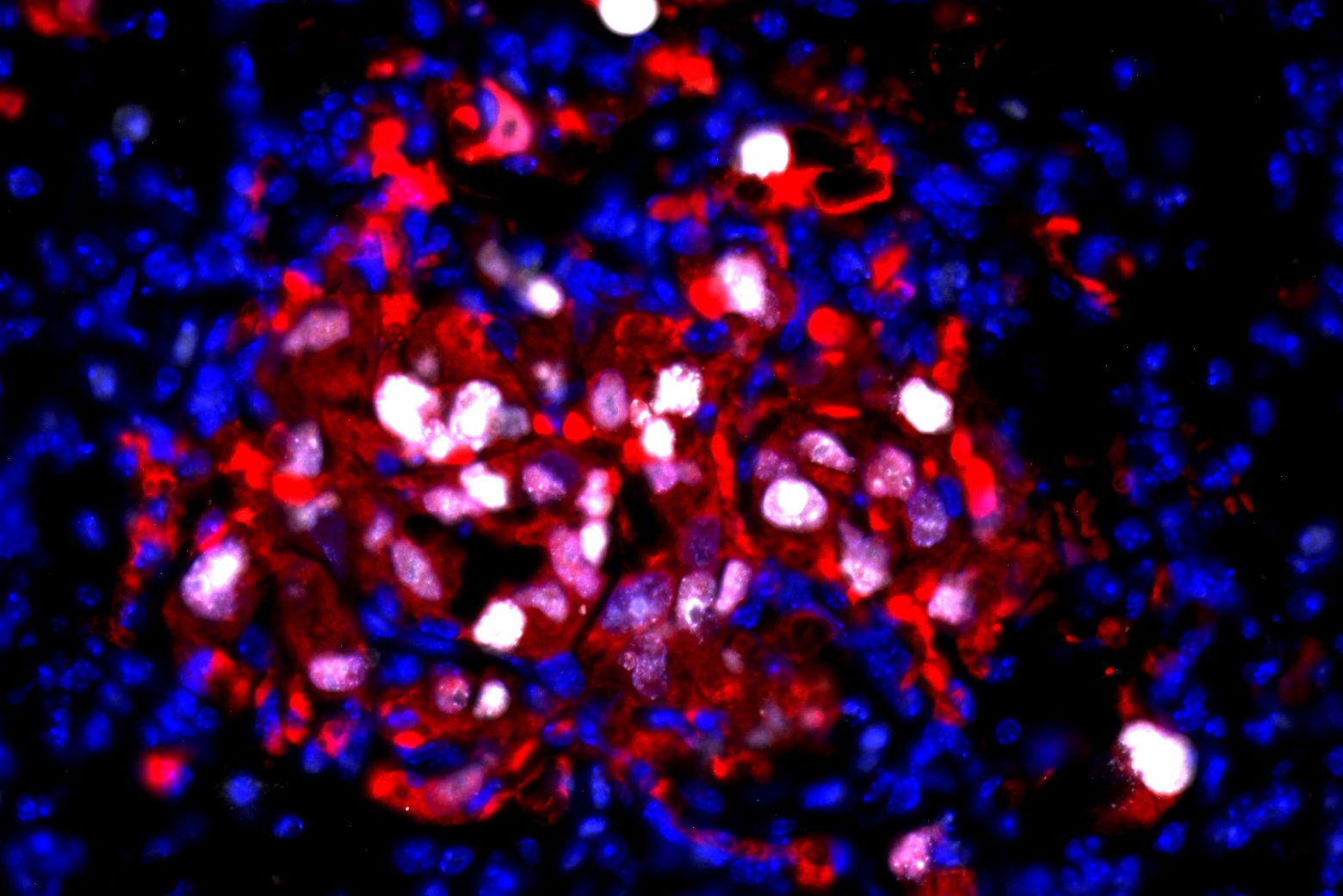
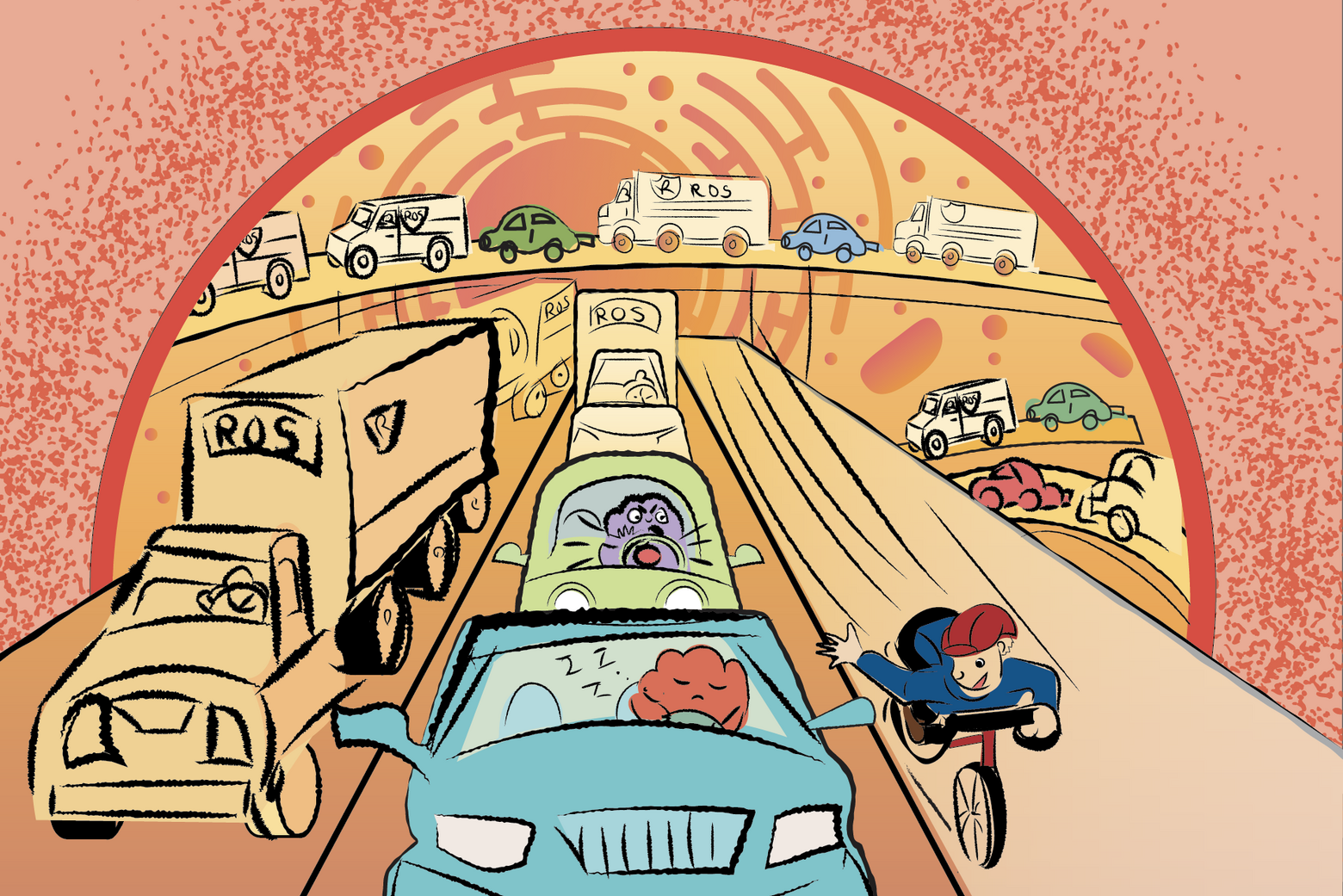
Further studies revealed that cysteine initiates a chain of events leading to the activation of a population of immune cells called CD8 T cells. When cells in the lining of the intestine absorb cysteine from digested food, they convert it into CoA, a cofactor that is released into the mucosal lining of the intestine. There, CD8 T cells absorb CoA, which stimulates them to begin proliferating and producing a cytokine called IL-22.
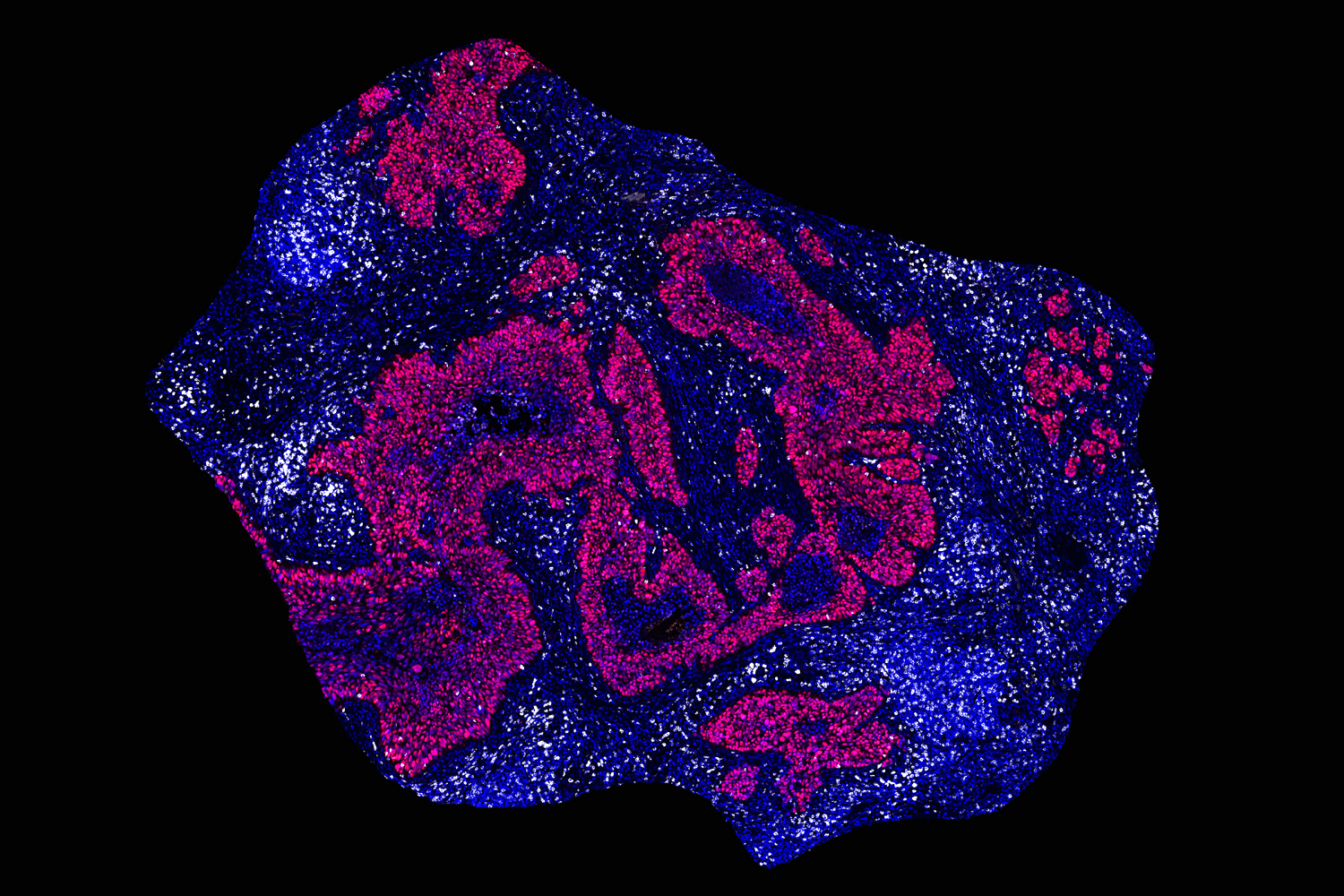
IL-22 is an important player in the regulation of intestinal stem cell regeneration, but until now, it wasn’t known that CD8 T cells can produce it to boost intestinal stem cells. Once activated, those IL-22-releasing T cells are primed to help combat any kind of injury that could occur within the intestinal lining.
“What’s really exciting here is that feeding mice a cysteine-rich diet leads to the expansion of an immune cell population that we typically don’t associate with IL-22 production and the regulation of intestinal stemness,” Yilmaz says. “What happens in a cysteine-rich diet is that the pool of cells that make IL-22 increases, particularly the CD8 T-cell fraction.”
These T cells tend to congregate within the lining of the intestine, so they are already in position when needed. The researchers found that the stimulation of CD8 T cells occurred primarily in the small intestine, not in any other part of the digestive tract, which they believe is because most of the protein that we consume is absorbed by the small intestine.
Healing the intestine
In this study, the researchers showed that regeneration stimulated by a cysteine-rich diet could help to repair radiation damage to the intestinal lining. Also, in work that has not been published yet, they showed that a high-cysteine diet had a regenerative effect following treatment with a chemotherapy drug called 5-fluorouracil. This drug, which is used to treat colon and pancreatic cancers, can also damage the intestinal lining.
Cysteine is found in many high-protein foods, including meat, dairy products, legumes, and nuts. The body can also synthesize its own cysteine, by converting the amino acid methionine to cysteine — a process that takes place in the liver. However, cysteine produced in the liver is distributed through the entire body and doesn’t lead to a buildup in the small intestine the way that consuming cysteine in the diet does.
“With our high-cysteine diet, the gut is the first place that sees a high amount of cysteine,” Chi says.
Cysteine has been previously shown to have antioxidant effects, which are also beneficial, but this study is the first to demonstrate its effect on intestinal stem cell regeneration. The researchers now hope to study whether it may also help other types of stem cells regenerate new tissues. In one ongoing study, they are investigating whether cysteine might stimulate hair follicle regeneration.
They also plan to further investigate some of the other amino acids that appear to influence stem cell regeneration.
“I think we’re going to uncover multiple new mechanisms for how these amino acids regulate cell fate decisions and gut health in the small intestine and colon,” Yilmaz says.
The research was funded, in part, by the National Institutes of Health, the V Foundation, the Koch Institute Frontier Research Program via the Kathy and Curt Marble Cancer Research Fund, the Bridge Project — a partnership between the Koch Institute for Integrative Cancer Research at MIT and the Dana-Farber/Harvard Cancer Center, the American Federation for Aging Research, the MIT Stem Cell Initiative, and the Koch Institute Support (core) Grant from the National Cancer Institute.