The substance that bathes tumors in the body is quite different from the medium used to grow cancer cells in the lab, biologists report.
Anne Trafton | MIT News Office
April 16, 2019
Before being tested in animals or humans, most cancer drugs are evaluated in tumor cells grown in a lab dish. However, in recent years, there has been a growing realization that the environment in which these cells are grown does not accurately mimic the natural environment of a tumor, and that this discrepancy could produce inaccurate results.
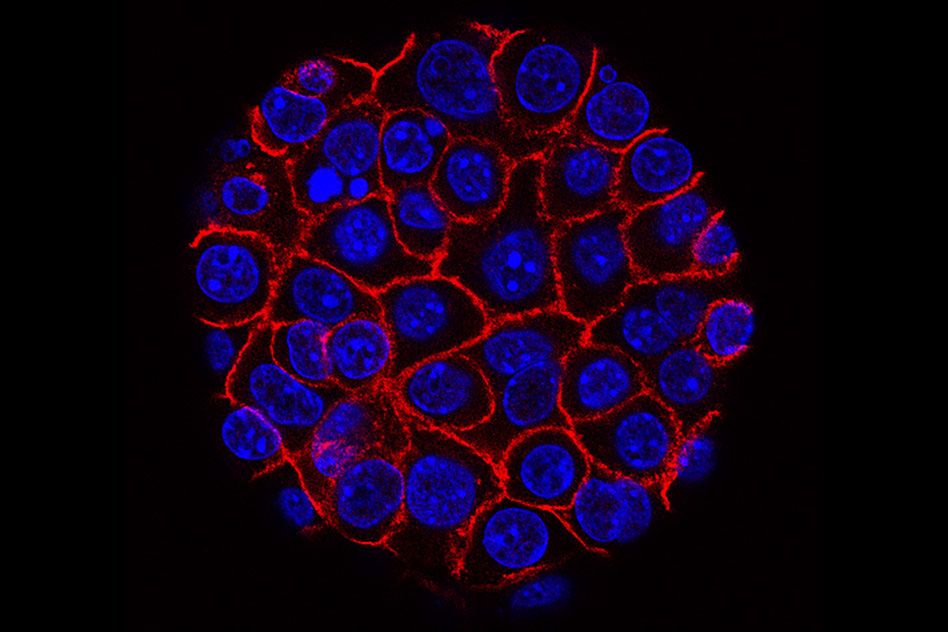
In a new study, MIT biologists analyzed the composition of the interstitial fluid that normally surrounds pancreatic tumors, and found that its nutrient composition is different from that of the culture medium normally used to grow cancer cells. It also differs from blood, which feeds the interstitial fluid and removes waste products.
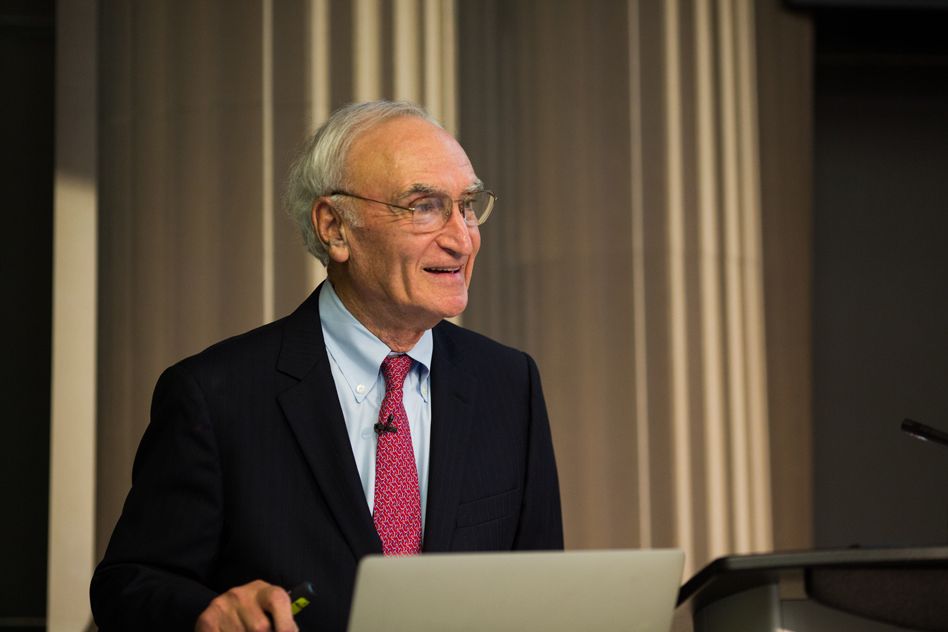
The findings suggest that growing cancer cells in a culture medium more similar to this fluid could help researchers better predict how experimental drugs will affect cancer cells, says Matthew Vander Heiden, an associate professor of biology at MIT and a member of the Koch Institute for Integrative Cancer Research.
“It’s kind of an obvious statement that the tumor environment is important, but I think in cancer research the pendulum had swung so far toward genes, people tended to forget that,” says Vander Heiden, one of the senior authors of the study.
Alex Muir, a former Koch Institute postdoc who is now an assistant professor at the University of Chicago, is also a senior author of the paper, which appears in the April 16 edition of the journal eLife. The lead author of the study is Mark Sullivan, an MIT graduate student.
Environment matters
Scientists have long known that cancer cells metabolize nutrients differently than most other cells. This alternative strategy helps them to generate the building blocks they need to continue growing and dividing, forming new cancer cells. In recent years, scientists have sought to develop drugs that interfere with these metabolic processes, and one such drug was approved to treat leukemia in 2017.
An important step in developing such drugs is to test them in cancer cells grown in a lab dish. The growth medium typically used to grow these cells includes carbon sources (such as glucose), nitrogen, and other nutrients. However, in the past few years, Vander Heiden’s lab has found that cancer cells grown in this medium respond differently to drugs than they do in mouse models of cancer.
David Sabatini, a member of the Whitehead Institute and professor of biology at MIT, has also found that drugs affect cancer cells differently if they are grown in a medium that resembles the nutrient composition of human plasma, instead of the traditional growth medium.
“That work, and similar results from a couple of other groups around the world, suggested that environment matters a lot,” Vander Heiden says. “It really was a wake up call for us that to really know how to find the dependencies of cancer, we have to get the environment right.”
To that end, the MIT team decided to investigate the composition of interstitial fluid, which bathes the tissue and carries nutrients that diffuse from blood flowing through the capillaries. Its composition is not identical to that of blood, and in tumors, it can be very different because tumors often have poor connections to the blood supply.
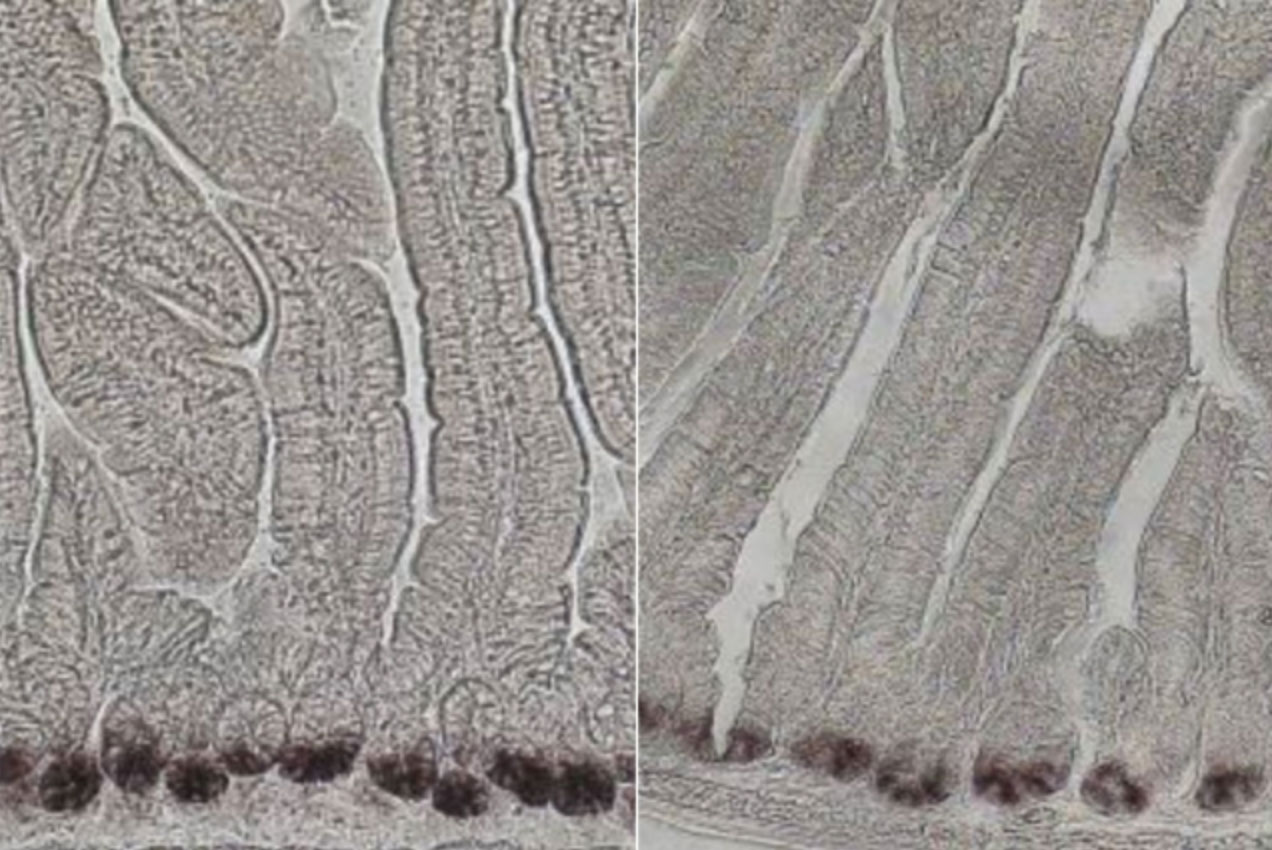
The researchers chose to focus on pancreatic cancer in part because it is known to be particularly nutrient-deprived. After isolating interstitial fluid from pancreatic tumors in mice, the researchers used mass spectrometry to measure the concentrations of more than 100 different nutrients, and discovered that the composition of the interstitial fluid is different from that of blood (and from that of the culture medium normally used to grow cells). Several of the nutrients that the researchers found to be depleted in tumor interstitial fluid are amino acids that are important for immune cell function, including arginine, tryptophan, and cystine.
Not all nutrients were depleted in the interstitial fluid — some were more plentiful, including the amino acids glycine and glutamate, which are known to be produced by some cancer cells.
Location, location, location
The researchers also compared tumors growing in the pancreas and the lungs and found that the composition of the interstitial fluid can vary based on tumors’ location in the body and at the site where the tumor originated. They also found slight differences between the fluid surrounding tumors that grew in the same location but had different genetic makeup; however, the genetic factors tested did not have as big an impact as the tumor location.
“That probably says that what determines what nutrients are in the environment is heavily driven by interactions between cancer cells and noncancer cells within the tumor,” Vander Heiden says.
Scientists have previously discovered that those noncancer cells, including supportive stromal cells and immune cells, can be recruited by cancer cells to help remake the environment around the tumor to promote cancer survival and spread.
Vander Heiden’s lab and other research groups are now working on developing a culture medium that would more closely mimic the composition of tumor interstitial fluid, so they can explore whether tumor cells grown in this environment could be used to generate more accurate predictions of how cancer drugs will affect cells in the body.
The research was funded by the National Institutes of Health, the Lustgarten Foundation, the MIT Center for Precision Cancer Medicine, Stand Up to Cancer, the Howard Hughes Medical Institute, and the Ludwig Center at MIT.