Most cells in our body live and die. But the germline, the cells that produce eggs and sperm, must carry on forever. How the germline successfully produces the next generation is a long-studied question. Through a string of discoveries made over years, the Yamashita lab is teasing apart how the germline remains immortal.
Madeleine Turner | Whitehead Institute
Most cells in our body live and die. But the germline, the cells that produce eggs and sperm, must carry on forever. How the germline successfully produces the next generation is a long-studied question. Research Threads examines how answering one question uncovers more questions to be solved. In our first installment of Research Threads, we follow the research of Whitehead Institute Member Yukiko Yamashita. Through a string of discoveries made over years, the Yamashita lab is teasing apart how the germline remains immortal.
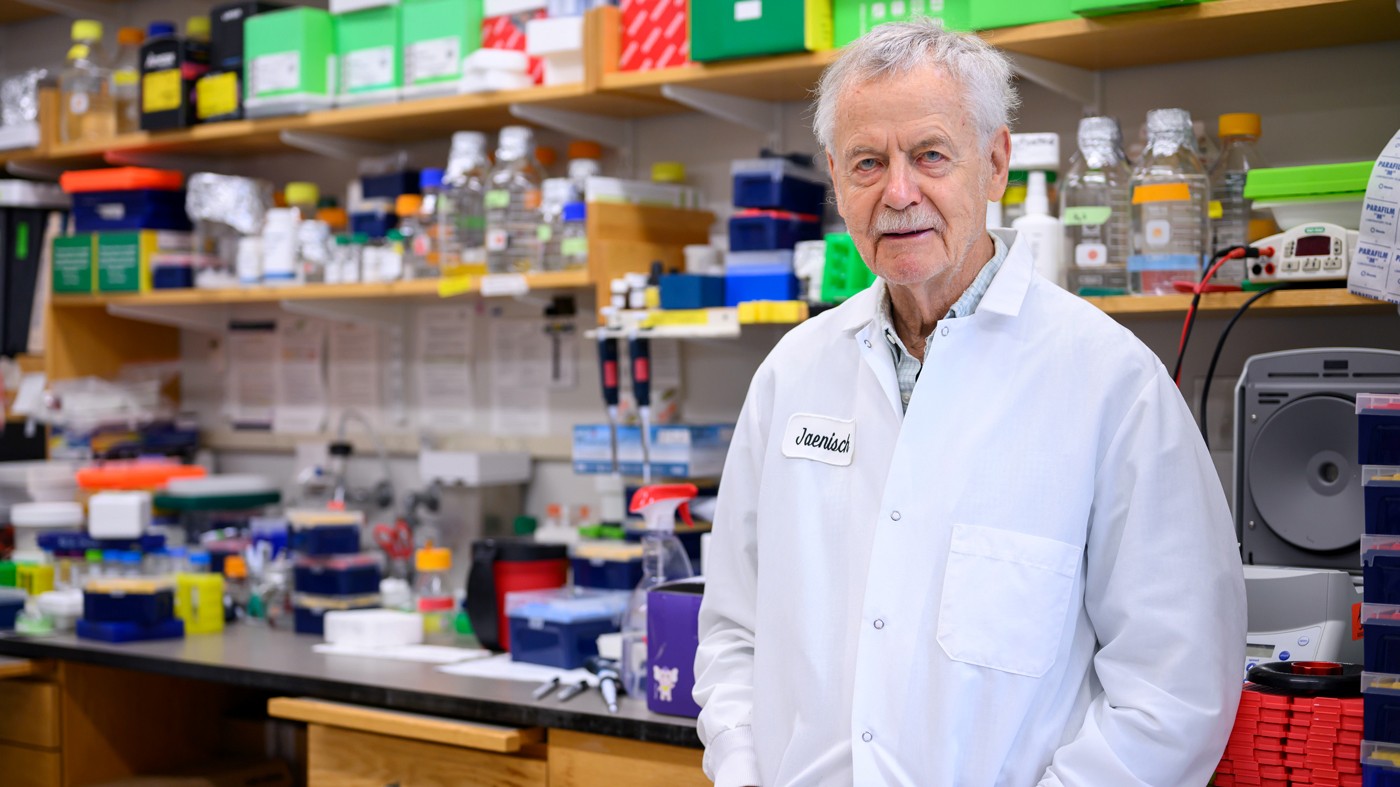
“The germline is the only cell type responsible for transmitting the genome from generation to generation,” Whitehead Institute Member Yukiko Yamashita says. “We’ve done that for 1.5 billion years.”
The germline is the population of cells in an organism that give rise to gametes, either egg or sperm cells. These gametes contain genetic information, encoded in DNA, needed to produce the next generation. The act of transmitting this information — the instructions that a new individual needs to develop and function — is like a relay race that never ends. While a skin or gut cell may be prone to genetic errors and is generally replaceable, germline stem cells (GSCs) must maintain their genomes with precision. Otherwise, any mistakes or imbalances would be inherited by offspring and accumulated over generations, potentially driving a species to extinction. In other words, to keep passing the baton in this relay, the germline must be faithfully preserved.
Although germline preservation is paramount to the existence and survival of a species, some fundamental parts of its biology have remained a mystery. Yamashita, who is also a professor of biology at the Massachusetts Institute of Technology and a Howard Hughes Medical Institute Investigator, has focused her research on unraveling the secrets of the germline. To study these cells’ immortality, her lab utilizes the model organism Drosophila melanogaster, or the fruit fly. Along the way, research in the Yamashita lab has highlighted how the process of scientific discovery can be circuitous, often pulling scientists in surprising directions, revealing new questions and avenues to explore.
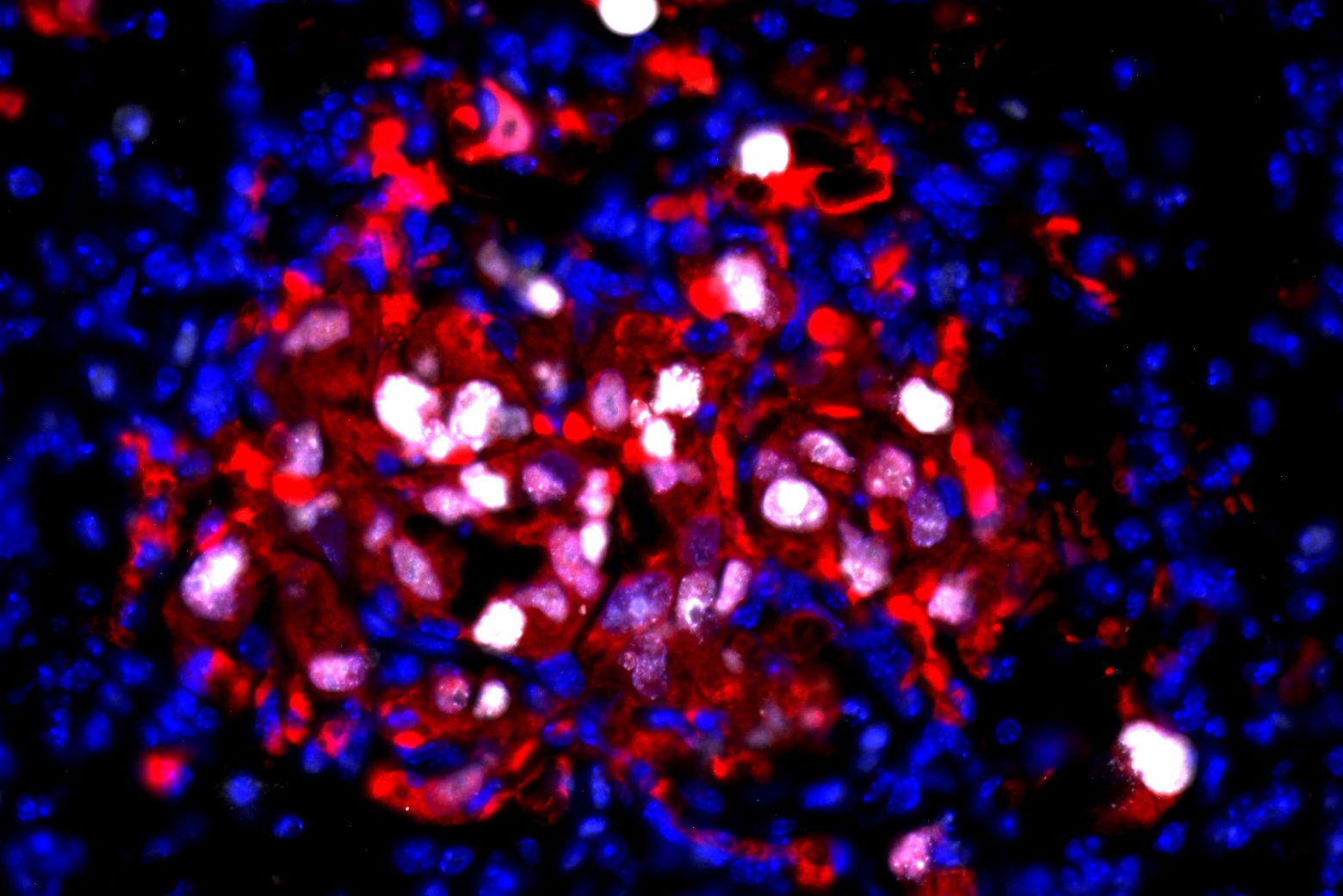
For decades, scientists had observed an aspect of germline behavior that was hard to explain. Most cells in the body divide to produce two identical copies, or daughter cells. GSCs in male fruit flies, however, divide “asymmetrically,” meaning they yield two daughter cells that are not identical. Instead, one daughter cell becomes a new GSC, while the other goes on to become a gamete, in this case a sperm cell. It might be easy to assume that asymmetric cell division is about producing gametes while maintaining a pool of stem cells. But an additional detail complicates this theory: when a daughter cell is on the path to becoming sperm, it can loop back around to become another stem cell, instead of continuing differentiation to become a sperm cell.
“If it can do that, why divide asymmetrically in the first place?” Yamashita says.
To shed light on why GSCs divide asymmetrically, researchers wanted to know how genetic information was actually divvied up between daughter cells. “After I started my own lab, there was this question hanging in the field,” Yamashita says. It made sense to find some difference in inheritance, DNA-based or otherwise: something to distinguish between the daughter fated to become a gamete, and the other that would remain in the GSC pool.
Preparing for division, a cell duplicates its DNA. Chromosomes happen to be shaped like the letter “X” as a result of this duplication: the left and right sides of the “X” are called matching sister chromatids, each a copy of the other. Later in cell division, these two sister chromatids part ways, winding up in separate daughter cells.
In 2013, Yamashita and her former graduate student, Swathi Yadlapalli, made a strange but important discovery. In fruit flies, for the X and Y chromosomes (the sex chromosomes), sister chromatids were not being sorted randomly. Instead, one was more likely to go to the daughter cell that would become a gamete; the other to the daughter on the GSC track. There had to be a reason for this preference, but no one had an explanation.
Initial experiments did not reveal obvious differences between these sister chromatid pairs. “Everyone would say, ‘oh, there’s probably some sort of epigenetic information in there,” Yamashita says, referring to heritable changes not carried in DNA. With few promising leads, the lab decided to take a systematic approach. George Watase, then a postdoc in the lab, began the painstaking work of removing different a parts of flies’ X chromosomes, seeing if the absence of any particular element would disrupt the pattern of preferential segregation.
“We thought it was going to be satellite DNA,” Yamashita says, referring to large swathes of DNA in the genome that are highly repetitive but don’t code for any genes. (While this initial guess was wrong, it kickstarted a separate project in the lab — one which led to discovering the unexpected role that satellite DNA plays when one species forks into two.)
Eventually the team narrowed in on the true culprit: ribosomal DNA (rDNA). The primary role of rDNA is to produce the components that make up ribosomes. Ribosomes, in turn, perform the crucial task of synthesizing proteins.
“We didn’t like this finding in the beginning. I always say that ribosomal DNA is ‘too important to be interesting.’ You don’t get excited about something you really need, like toilet paper,” Yamashita says. “In the case of ribosomal DNA, bacteria needs it, humans need it, everybody needs it.”
But what did rDNA have to do with asymmetric cell division in the germline?
“Around that time, we started reading lots of papers,” Yamashita says. “Then we discovered a phenomenon called rDNA magnification. These were studies from the 1960s and ’80s — most of the people in my lab were not even born yet.”
These studies from decades ago described mutant flies that lacked a sufficient amount of rDNA and, as a result, had a “bobbed” phenotype, or appearance. Since these flies possessed fewer ribosomes to produce proteins, the bristles on their back were shorter; the protective cuticle covering their bodies weakened. But when they reproduced, many of their offspring possessed a normal amount of rDNA. These observations pointed towards a mechanism that allowed flies to replenish their supply of rDNA.
At the time rDNA magnification was first observed, the phenomenon was regarded as an oddity, something that only happened in mutant flies and did not have physiological relevance. But Yamashita realized there was a connection between rDNA magnification and asymmetric division in the germline.
To make enough protein, a cell must produce ample ribosomes. To do that, the fruit fly genome contains hundreds of copies of rDNA in a row. But the DNA replication process can struggle to handle so many rDNA copies strung together, and can sometimes experience a hiccup, resulting in the loss of rDNA copies with each new division. It’s an outcome that might be okay on occasion, but would wreak havoc over many generations.
“All of a sudden, [rDNA magnification] was not about a mutant chromosome,” Yamashita says. “We were like, holy moly. This is about germline immortality.”
Soon many different pieces became part of a cohesive story: asymmetric cell division is not about producing a balance of gametes and stem cells; it’s about maintaining rDNA in the germline. Sister chromatids are almost identical — but one contains more copies of rDNA than the other, and that copy is fated to stay in the GSC pool. Through this asymmetry, the germline is replenished of rDNA; it can pass the baton to the next generation.
“For quite some time, for so many observations that everyone knew in the field, we felt we had an explanation. But from that ‘aha!’ moment, we took multiple years to test everything,” Yamashita says.
In subsequent years, the Yamashita lab pinned down additional details about how rDNA is diverted back to the germline. First, in 2022, the team identified a specific protein, which they named Indra, which binds to rDNA. The presence of Indra helps assign the sister chromatid containing more rDNA copies to the GSC daughter cell.
Their next discovery was another plot twist. If one sister chromatid contained more rDNA than the other, and those rDNA copies weren’t appearing out of thin air, it meant that one chromatid needed to be stealing rDNA from its sister. The lab discovered a genetic element that facilitated this transfer: a retrotransposon.
Retrotransposons are usually considered “genetic parasites,” copying and pasting themselves into the genome. In an attempt to reinsert itself, this particular retrotransposon, called R2, slices open sections containing rDNA on both chromatids. As the cell repairs these breaks, it may inadvertently stitch copies of rDNA from one chromosome to the other, creating an unequal number of copies between the two.
“Not many people thought retrotransposons could be beneficial to the host. They’re seen as parasites,” Yamashita says. “But it turns out that they are essential for germline immortality.”
Sometimes, one research project is a spin off of a spin off. That was true for Xuefeng Meng, a graduate student in the lab who was working on satellite DNA, the genetic element that turned out to be unrelated to asymmetric cell division, but was interesting in its own right.
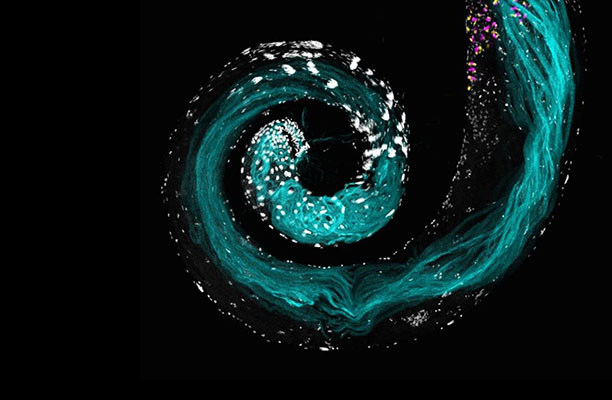
While studying satellite DNA, Meng noticed that a particular stock of flies had a problem producing normal sperm, that their cells’ nuclei were abnormally packaged. The problem had to do with a gene called Stellate on the flies’ X chromosome. While most flies have few copies of Stellate, these flies had a higher number of copies.
Stellate was already known in the field as a meiotic driver, or “selfish-gene”: a genetic element that has evolved ways to preferentially transmit itself to the next generation. Some meiotic drivers, including Stellate, are on the sex chromosomes and, when not suppressed, cause an excess of either male or female progeny. In this case, Stellate produces a protein, Ste, which is found to concentrate in Y-carrying cells during meiosis, the specialized type of cell division that produces gametes (meiosis follows the earlier round of asymmetric cell division described above). High concentrations of Ste impede the proper packaging of nuclei in cells, leading to their eventual death. When Stellate is widely expressed, fewer male flies emerge in the next generation.
But here lies an inherent tension: if a selfish gene is too good at propagating itself, and produces only males or females, its host species would go extinct — and so would the gene. Meng and Yamashita were interested in this paradox. Through this work, they
identified a novel mechanism that keeps Stellate in check. To balance selfish propagation with the host species’ survival, Stellate has a built-in system for pumping the brakes. After Ste concentrates in Y-carrying cells during the first meiotic division, the protein is unevenly distributed a second time. This second step spares a portion of Y-carrying cells that go on to create males.
How the germline is able to counter disruptive forces, thereby renewing itself, continues to be a ripe research area. Researchers still don’t know all the secrets to how a line of cells can achieve perpetuity — but the Yamashita lab continues to investigate the question.
“What I really like about people in my lab is that they don’t jump to the easiest conclusion,” Yamashita says. “If you start embracing surprise, then good things happen. Because you are surprised, you start testing your finding in multiple ways. Then you can build confidence about the result.”
Notes
Xuefeng Meng and Yukiko Yamashita (2025). “Intrinsically weak sex chromosome drive through sequential asymmetric meiosis.” Science Advances. https://doi.org/10.1126/sciadv.adv7089
Jonathan O. Nelson, Tomohiro Kumon, Yukiko M. Yamashita. (2023) “rDNA magnification is a unique feature of germline stem cells.” PNAS. https://doi.org/10.1073/pnas.2314440120
Jonathan O. Nelson, Alyssa Slicko, Yukiko M. Yamashita. (2023) “The retrotransposon R2 maintains Drosophila ribosomal DNA repeats.” PNAS. https://doi.org/10.1073/pnas.2221613120
George J. Watase, Jonathan O. Nelson, Yukiko M. Yamashita. (2022) “Nonrandom sister chromatid segregation mediates rDNA copy number maintenance in Drosophila.” Science Advances. https://www.science.org/doi/10.1126/sciadv.abo4443
Madhav Jagannathan and Yukiko Yamashita. (2021) “Defective satellite DNA clustering into chromocenters underlies hybrid incompatibility in Drosophila.” Molecular Biology and Evolution. https://doi.org/10.1093/molbev/msab221
Swathi Yadlapalli and Yukiko Yamashita (2013) “Chromosome-specific nonrandom sister chromatid segregation during stem-cell division.” Nature. 10.1038/nature12106