Eva Frederick | Whitehead Institute
April 20, 2020
In overgrown areas from Canada to China, a lush, woody vine with crescent-shaped seeds holds the secret to making a cancer-fighting chemical. Now, Whitehead Institute researchers in Member Jing-Ke Weng’s lab have discovered how the plants do it.
Plants in the family Menispermaceae, from the Greek words “mene” meaning “crescent moon,” and “sperma,” or seed, have been used in the past for a variety of medicinal purposes. Native Americans used the plants to treat skin diseases, and would ingest them as a laxative. Moonseed was also used as an ingredient in curare, a muscle relaxant used on the tips of poison arrows.
But the plants also may have a use in modern-day medicine: a compound called acutumine shown to have anti-cancer properties (although not tested specifically against cancer cells, the chemical has been shown to kill human T-cells, an important quality for leukemia and lymphoma treatments). Acutumine is a halogenated product, which means the molecule is capped on one end by a halogen atom — a group that includes fluorine, chlorine and iodine, among others. In this case, the halogen is chlorine.
Halogenated compounds like acutumine can be useful in medicinal chemistry — their unusual chemical appendages mean they react in interesting ways with other biomolecules, and drug designers can put them to use in creating compounds to complete specific tasks in the body. Today, 20% of pharmaceutical compounds are halogenated. “However, chemists’ ability to efficiently install halogen atoms to desirable positions of starting compounds has been quite limited,” Weng says.
Most natural halogenated products come from microorganisms such as algae or bacteria, and acutumine is one of the only halogenated products made by plants. Chemists finally succeeded in synthesizing the compound in 2009, although the reaction is time-consuming and expensive (10 mg of synthesized acutumine can cost around $2,000).
Colin Kim, a graduate student in the Weng lab at Whitehead Institute, wanted to know how these plants were completing this tricky reaction using only their own genetic material. “We thought, why don’t we ask how the plants make it and then upscale the reaction [to produce it more efficiently]?” Kim says.
“By understanding how living organisms such as the moonseed plant perform chemically challenging halogenation chemistry, we could devise new biochemical approaches to produce novel halogenated compounds for drug discovery,” Weng says.
Kim knew that for every halogenated molecule in an organism, there is an enzyme called a halogenase that catalyzes the reaction that sticks on that halogen. Halogenases are useful in creating pharmaceuticals – a well-placed halogen can help fine-tune the bioactivities of various drugs. So Weng, who is also an associate professor of biology at Massachusetts Institute of Technology, and Kim, who spearheaded the project, began working to identify the helper molecule responsible for creating acutumine in moonseed plants.
First, the scientists obtained three species of Menispermaceae plants. Two of them, common moonseed (Menispermum canadense) and Chinese moonseed (Sinomenium acutum), were known to produce acutumine. They also procured one plant in the same family called snake vine (Stephania japonica) which did not produce the compound.
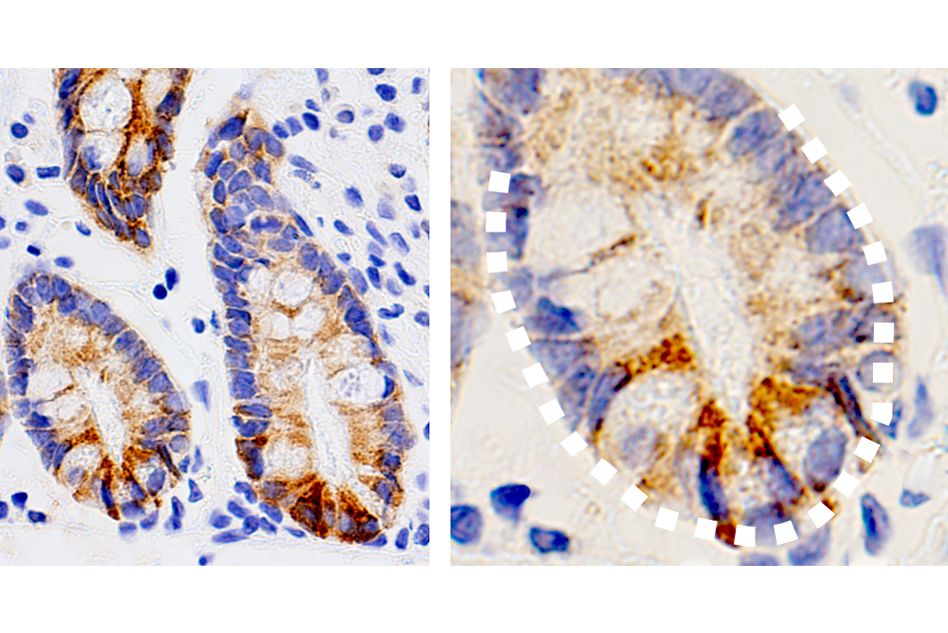
They began their investigation by using mass spectrometry to look for acutumine in all three plants, and then find out exactly where in the plants it was located. They found the chemical all throughout the first two — and some extra in the roots of common moonseed. As expected, the third plant, snake vine, had none, and could therefore be used as a reference species, since presumably it would not ever express the gene for the halogenase enzyme that could stick on the chlorine molecule.
Next, the researchers started searching for the gene. They began by sequencing the RNA that was being expressed in the plants (RNA serves as a messenger between genomic DNA and functional proteins), and created a huge database of RNA sorted by what tissue it had been identified in.
At this point, the extra acutumine in the roots of common moonseed came in handy. The researchers had some idea of what the enzyme might look like – past research on other halogenases in bacteria suggested that one specific family of enzyme, called Fe(II)/2-oxoglutarate-dependent halogenases, or 2ODHs, for short, was capable of site-specifically adding a halogen in the same way that the moonseed’s mystery enzyme did. Although no 2ODHs had yet been found in plants, the researchers thought this lead was worth a look. So they searched specifically for transcripts similar to 2ODH sequences that were more highly expressed in the roots of common moonseed than in the leaves and stems.
After analyzing the RNA transcripts, Kim and Weng were pretty sure they had found what they were looking for: one gene in particular (which they named McDAH, short for M. canadense dechloroacutumine halogenase) was highly expressed in the roots of common moonseed. Then, in Chinese moonseed, they identified another protein that shared 99.1 percent of McDAH’s sequence, called SaDAH. No similar protein was found in snakevine, suggesting that this protein was likely the enzyme they wanted.
To be sure, the researchers tested the enzyme in the lab, and found that it was indeed the first-ever plant 2ODH, able to stick on the chlorine molecule to the alkaloid molecule dechloroacutumine to form acutumine. Interestingly, the enzyme was pretty picky; when they gave it other alkaloids like codeine and berberine to see if it would install a halogen on those as well, the enzyme ignored them, suggesting it was highly specific toward its preferred substrate, dechloroacutumine, the precursor of acutumine. They compared the enzyme’s activity to other similar enzymes, and found the key to its ability lay in the substitution of one specific amino acid in the active site– aspartic acid — for a glycine.
Now that they had identified the enzyme responsible for the moonseed’s halogenation reactions, Kim and Weng wanted to see what else it could do. A chemical capable of catalyzing such a complex reaction might be useful for chemists trying to synthesize other compounds, they hypothesized.
So they presented the enzyme with some dechloroacutumine and a whole buffet of alternative anions to see whether it might catalyze a reaction with any of these molecules in lieu of chlorine. Of the selection of anions, including bromide, azide, and nitrogen dioxide, the enzyme catalyzed a reaction only with azide, a construct of 3 nitrogen atoms.
“That is super cool, because there isn’t any other naturally occurring azidating enzyme that we know of,” Kim says. The enzyme could be used in click chemistry, a nature-inspired method to create a desired product through a series of simple, easy reactions.
In future studies, Weng and Kim hope to use what they’ve learned about the McDAH and SaDAH enzymes as a starting point to create enzymes that can be used as tools in drug development. They’re also interested in using the enzyme on other plant products to see what happens. “Plant natural products, even without chlorines, are pretty effective and bioactive, so it would be cool to see if you can take those plant natural products and then install chlorines to see what kind of changes and bioactivity it has, whether it develops new-to-nature functions or retain its original bioactivity with enhanced properties,” Kim says. “It expands the biocatalytic toolbox we have for natural product biosynthesis and its derivatization.”
***
Written by Eva Frederick
***
Citation: Kim, Colin Y. et al. The chloroalkaloid (−)-acutumine is biosynthesized via a Fe(II)- and 2-oxoglutarate-dependent halogenase in Menispermaceae plants. Nature Communications. April 20, 2020. DOI: 10.1038/s41467-020-15777-w