Eva Frederick | Whitehead Institute
October 25, 2021
Many people — around half of the adult population — are infected with a type of herpesvirus called human cytomegalovirus, or HCMV. Though mostly asymptomatic, the virus can be dangerous for immunocompromised people and unborn babies. Because HCMV is so widespread, the chance of a baby becoming infected in utero is around one in 200, and that infection can lead to problems with the baby’s brain, lungs and growth.
In a new paper from Whitehead Institute Member Jonathan Weissman published on October 25 in Nature Biotechnology, Weissman and colleagues turn cutting-edge CRISPR and single cell sequencing technologies on this virus, providing the most detailed picture yet on how viral and human genes interact to create an HCMV infection — and revealing new ways to potentially derail the virus’ progression through manipulating viral and host genes.
The research could provide an important road map for future studies of host-pathogen interactions, as well as inform antiviral drug design. Over the course of the project, the researchers generated a list of both viral and host genes that were either essential for the virus to replicate, or could potentially be manipulated to confer some immunity to the host cell. “Now that we have this list, we have a list of potential targets that one might now go ahead and develop drugs against,” said Marco Hein, the first author and a former postdoctoral researcher in the Weissman Lab.
Seeing both sides
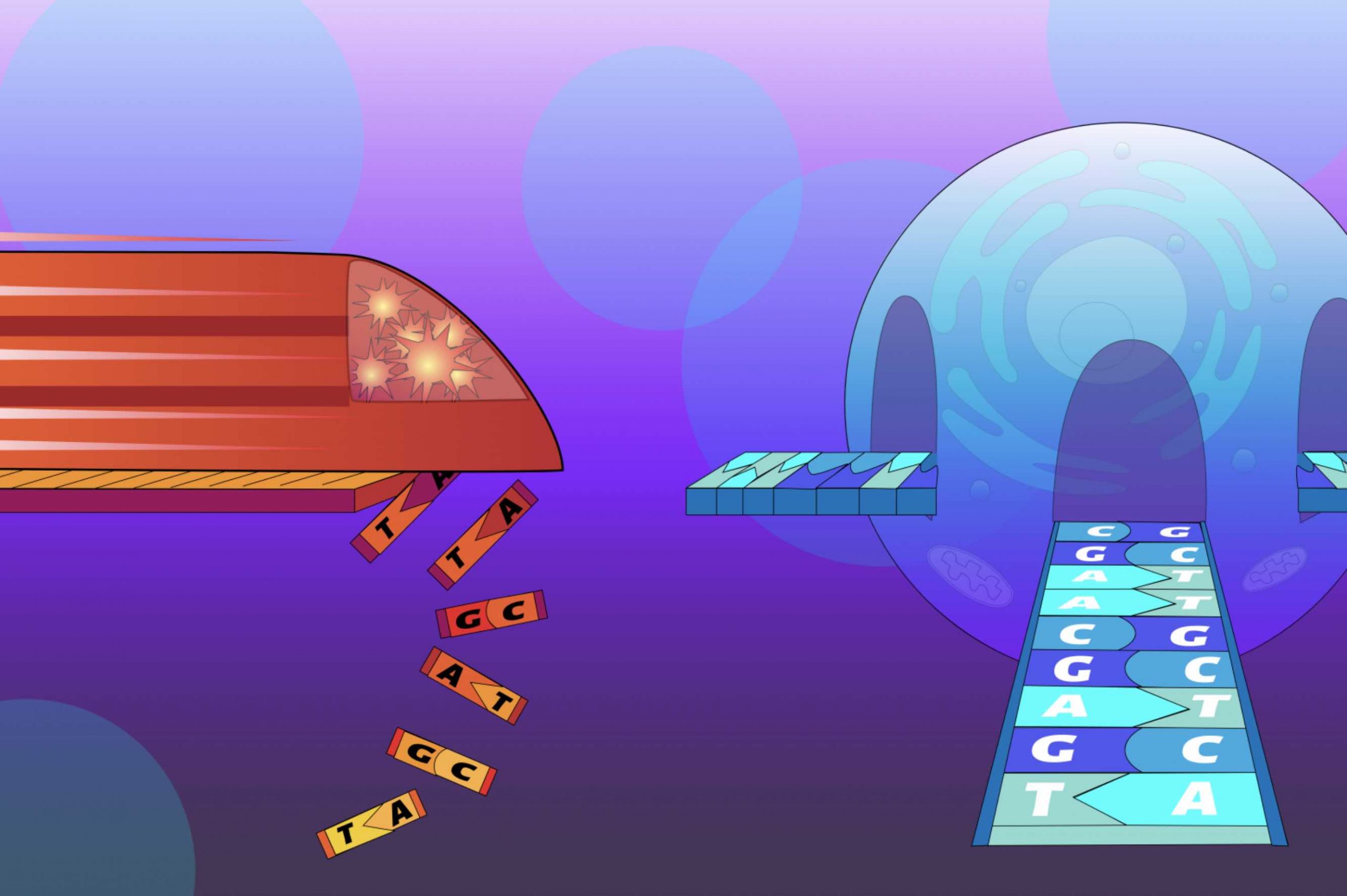
Millions of years of evolution have created a complex web of interactions between virus and host. For example, viruses have their own set of genes, but they also depend on some human genes, called host factors. Hijacking these host factors allows the viruses to invade cells in the body and replicate their own genetic material.
Hein, who is now a researcher at the Chan Zuckerberg Biohub in San Francisco, and Whitehead Institute Member Jonathan Weissman, who is also a professor of biology at the Massachusetts Institute of Technology and Koch Institute and an investigator of the Howard Hughes Medical Institute, sought to gain a more thorough understanding of the web of host-viral interactions that arises throughout the course of an infection. “[We wanted to know] what actually happens when we [knock out or weaken] those critical factors,” Hein said. “Can we prevent infection? If so, what ‘goes wrong’ from the perspective of the virus?”
They chose HCMV as a test subject because, for one thing, the virus has a double-stranded DNA genome like humans. That means that CRISPR technologies that work by snipping DNA could theoretically work for both the virus and the host. “And because CMV is an important human pathogen and it’s such a complex and intricate virus, we thought we would have a chance to really discover something new,” said Weissman.
A series of screens
The researchers first set out, using a molecular technique called CRISPR screening, to determine whether any regions of the viral or host genomes in particular had an impact on the fate of infected host cells. By systematically knocking out individual genes in a large population of viruses and host cells, the researchers could then assess how essential each gene was to the infection.
The project took on a new dimension in 2016 with the development of accessible, large-scale single cell sequencing. “We had this idea to put together the CRISPR screening and the single cell sequencing, and [a screening method called PerturbSeq],” Hein said. “Basically, you perturb genes in a cell population and then you read out what happens to the cells, not just by measuring survival, but by actually looking at the pattern of gene expression in those cells over time.”
Combining these methods generated a huge set of data, which provided the researchers with a clearer view of which genes were important and when. “The single cell sequencing lets us watch the steps in the viral life cycle with much higher precision, and then the perturbation lets us understand how host and viral factors allow the virus to manipulate the host and complete its life cycle,” Weissman said.
The resultant data showed how the virus’ typical trajectory — from the initial waves of viral gene expression, to replication of the full viral genome, to the final step of budding off into newly-formed virions — could be derailed by altering specific viral genes. It also clued the researchers in to which host genes the virus depended on at what stages for a ‘successful’ infection.
“The course of infection is pre-programmed into the viral genome,” Hein said. “If you want to interfere with the course of infection you can do that by targeting a viral factor, or you can do it indirectly by targeting the host factor. And the outcomes are conceptually different. If you target a virus factor you derail the program that the virus would normally follow. If you target a host factor, the program itself is unchanged, but you change how far the virus gets in executing the program.”
These findings will be useful tools for the development of drugs that can be used as part of an antiviral “cocktail.” Because viruses and other pathogens are living creatures that can mutate and adapt to changing conditions, a common thread among antiviral treatments involves combining several drugs with different viral targets. This ensures the most complete eradication of viruses possible, reducing the chance that some will survive and create a new resistant population.
While the researchers’ list of essential viral genes provide parts of HCMV to target with drug cocktails, the list of contributing human genes could open the door for a more indirect therapy. “If you target a host factor to affect the virus, it’s much more difficult for the virus to escape because it can’t just mutate so the drug doesn’t bind anymore — it would have to mutate away from dependency on a host protein, which is much more complicated,” Hein said.
Of course, there are drawbacks to potentially targeting a human gene or protein to treat an infection, and much more work would need to be done for a viable treatment to emerge via this avenue of research. “If you target a host factor, you’re by definition targeting a protein that’s in our body, doing its normal job, so the risk of side effects is much higher,” Hein said.
Few drugs like this have made it past clinical trials; one famous example is hydroxychloroquine, which has been used successfully to treat malaria, and unsuccessfully to treat COVID-19.
In the future, Hein and Weissman hope to turn their multi-level approach for studying infection toward other viruses such as SARS-CoV-2. Although the novel coronavirus does not have double-stranded DNA that can be altered via CRISPR, the researchers can still investigate which host genes are essential at what stage of infection, and use their methods-driven approach to hopefully glean unexpected findings from a well-studied virus.
“I’m always driven by what technology can do,” Hein said. “I like to run a study in a systems-wide manner and then come up with some findings that you would have not found if you had only looked at one gene or protein at a time or looked at things more in the conventional way. This kind of high-level conclusion is what I personally always find the most exciting.”
